Sciatica is not a “disease” in and of itself. “Sciatica” simply describes a set of symptoms that can be caused by a number of conditions. For that reason, it is very sensible to ask the question “Which type of sciatica do I have?”
Sciatica is a tricky problem, as many conditions can cause sciatica. To complicate matters further, there are many conditions which mimic the symptoms of sciatica, making it even harder to identify what is causing your pain.
As with any condition or pain you are experiencing, it is important to identify the root cause of the problem to map out an effective treatment plan.
This article aims to do the following:
- Describe some of the most common conditions which cause sciatica and help you answer the question “Which type of sciatica do I have?”
- Outline treatment options for each condition
- Briefly touch upon some of the conditions which mimic the effects of sciatica
Before we begin, let’s take a moment to identify some of the key anatomical structures involved in these conditions.
Despite sciatica often causing pain which radiates through the buttock(s) and leg(s), the problem typically stems from the spine.
The spine is made up of 24 movable bones called vertebrae. Each of these bones are separated by an intervertebral disc – a tough sac made of strong cartilage, filled with fluid. The outer layer is called the annulus fibrosus, which holds a jelly-like centre called the nucleus pulposus. These discs act as cushions to absorb the impact of movement and prevent the vertebrae from grinding against each other.
The spine not only functions to provide structure for our body, offering support for the body to complete movement, but it is also responsible for housing the spinal cord. This “house” is called the spinal canal – a tunnel through the spine whereby the spinal cord runs. The spinal cord runs from your brain all the way down to the bottom of your back, supplying nerves throughout your entire body.
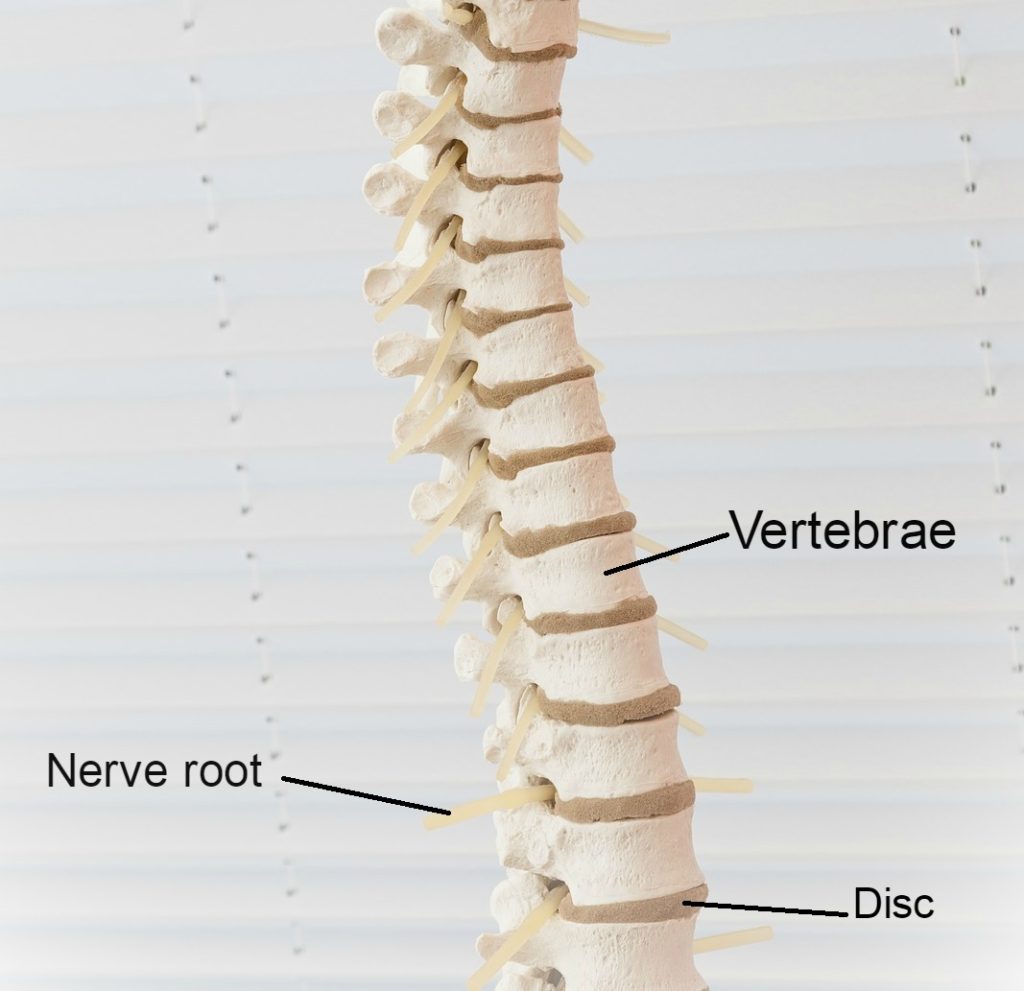
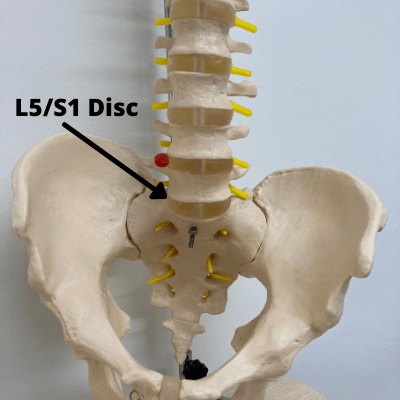
Your lower back, called the lumbar spine, is made up of 5 large lumbar vertebrae. These are called L1 to L5; with L5 being the lowest vertebra in the spine. We name these discs based on the vertebrae above and below the disc. For example, if we are talking about the disc between L4 and L5, we would call it disc L4/L5.
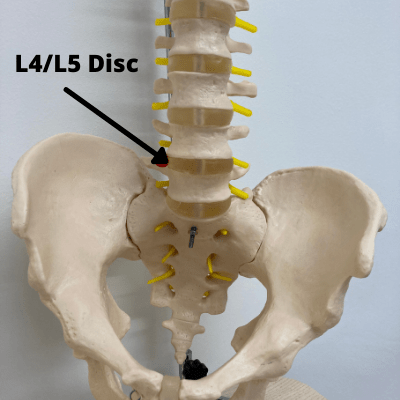
Our lumbar spine supplies the nerves to our legs. Damage to this area is common, given our lumbar area is one of our most frequently recruited sites for movement. Because of the way our spines are designed, they have special curves at the top, middle and bottom. When we walk and move, the areas that have a more dramatic curve tend to suffer from more stress than the areas that don’t curve.
Your sciatic nerve is the largest in the body, running from your lower back and down through your legs. Compression or irritation of the sciatic nerve roots can cause the pain known as sciatica – typically a sharp, shooting pain that may prevent you from being able to perform much movement.
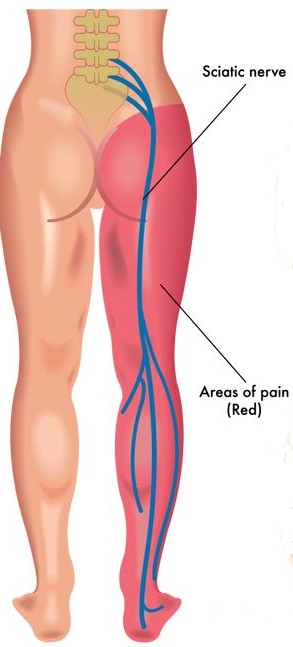
Because of the length of the sciatic nerve, the pain may run from your back into your buttock and all the way down one leg. Because your sciatic nerve is responsible for sending messages and relaying feeling down your legs, issues with the spine often cause pain, aching or distorted sensation along this pathway, rather than at the nerve root.
Now, let’s have a look at some of the most common conditions which cause sciatica, to help you identify what type of sciatica you may have.
#1 Disc Bulge or Herniated Disc
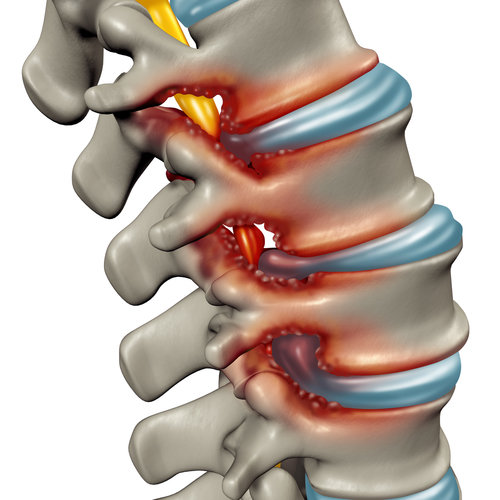
A disc bulge does what it says on the tin – one or more of the discs bulges outwards from its usual place in between two vertebrae. When the disc protrudes outwards, it can press against the spinal nerve roots.

The above picture shows a bulging disc pressing against the nerve root (the yellow stem) as it exits the spine (this gap is called the foramen).
Touching, pinching, or compressing a nerve causes reactions around that area, causing pain along the entire course of the nerve. You will get sciatica symptoms from the direct contact but also a chemical reaction around that area which exacerbates these symptoms. The chemical reaction that occurs when we compress a nerve, especially when part of a spinal disc touches the sciatic nerve, is similar to the type of reaction we get when we are stung by a bee.
If one part of the disc has weakened significantly more than others, it can lead to something called a herniated disc. This describes the event whereby the strong outer fibres of the disc split (or “herniate”) and the fluid within the disc leaks out at the region where the injury occurred. This is different from a bulging disc, whereby the outer layer remains intact enough to contain the centre (nucleus pulposus).
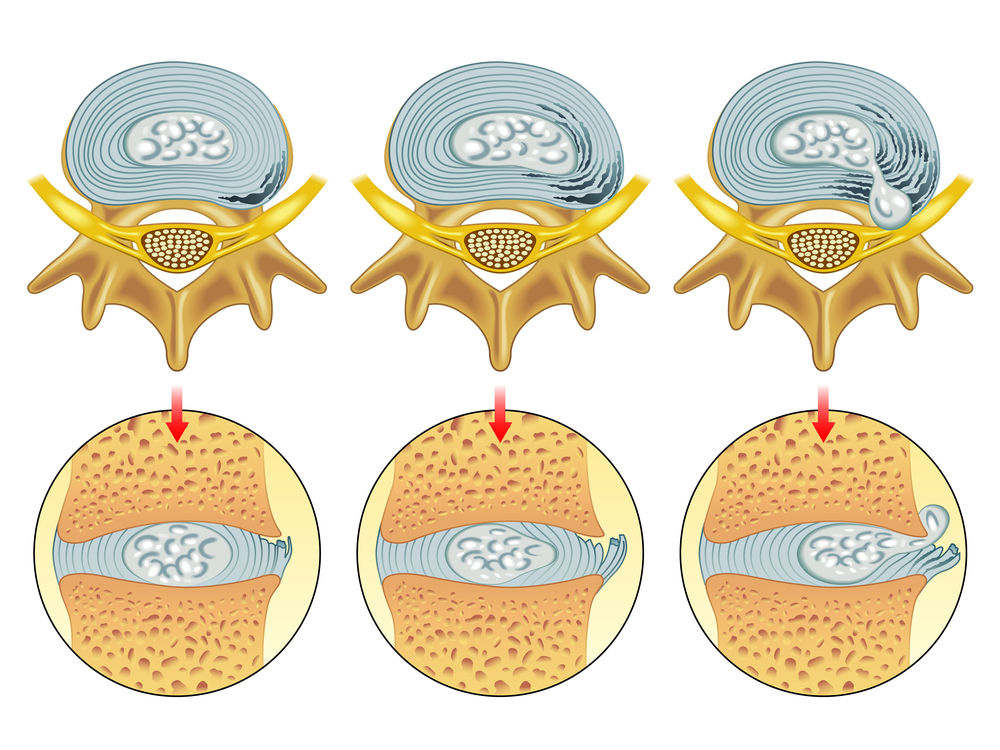
The above shows different degrees of disc damage. The left-hand and middle image show bulging discs, whilst the right-hand image shows a herniated disc.
A herniated disc is more likely than a bulging disc to cause sciatica, as the disc protrudes further, making it more likely to affect the surrounding nerve roots. However, the severity of the injury does not necessarily reflect the severity of the symptoms.
Learn more about how a bulging or herniated disc causes symptoms using the video below:
A herniated disc is an extremely common problem. So common, in fact, that 1 in 10 people will suffer from sciatica at some point in their lives and the vast majority of those cases are caused by a herniated disc.
If someone suffers from a herniated disc at L5/S1 (where the lumbar spine and sacrum meet), a disc which is extremely close in proximity to the sciatic nerve, the inner material from the disc often touches the nerve and can cause L5/S1 nerve root compression symptoms, which include sciatica, numbness, and weakness in the leg. A herniated L5/S1 disc is one of the most common injuries I see when treating sciatica.
With an injury at L5-S1, there is often a typical L5-S1 pain pattern. The pattern will depend on whether the L5 nerve root is affected, or whether the S1 nerve root is affected, or both.
The L5 pain pattern involves pain running down the OUTSIDE of the leg to the outer shin and then running to the outside border of the foot. The S1 pain pattern is more like “classic sciatica” with pain running directly down the back of the leg, often all the way into the toes.
How to treat it
With a herniated disc, treatment should always be guided by a qualified healthcare professional, due to the complexities of the injury. The following should not be taken as medical advice, rather as a rough guide to what I find has worked as the most effective treatment for a herniated disc. Below are my top tips for speeding up disc recovery and fight off your sciatica.
- Diet: It’s crucial that diet is optimised to speed up disc recovery. For the ideal recovery diet, you want to increase anti-inflammatory and decrease inflammatory food. Click each link to for information on which foods to stock up on and which foods to avoid.
- Activity: Most people do best when they keep generally active after a herniated disc L5/S1. This means not taking too much time off work to prevent further damage or general weakening of the body from inactivity. Most people should try to walk as much as they can within the realms of comfort. The best advice is to stop when pain starts, have a break, then get back to it.
- Hydration: Drinking plenty of water is a highly undervalued facet of recovery, as any dehydration in the injured disc will make the nerve compression worse. Drinking 3-4 litres of water each day is critical for recovery.
- Sleep: Getting as much sleep as possible is incredibly important when you have a herniated disc L5/S1 (although, sciatica can make sleep more difficult, unfortunately). Sleep is one of the key parts of a recovery from a herniated disc L5/S1 – sleep is when healing occurs. It’s nearly impossible to get better without ample sleep each night. If you’re struggling with sleeping, please check out my tips to help you get a better night’s sleep.
Everyone is different and it is difficult to tell who is going to improve very quickly, and who will have a longer recovery time. What’s even more confusing is that the severity of the disc herniation is NOT a good predictor of herniated disc recovery time!
However, as a rough guideline I would expect a recovery to follow this pattern in an absolutely “typical” individual:
| When? | Stage of Recovery |
| Day 1 | Disc injury occurs – severe symptoms! |
| Week 1 | In lots of pain, struggling to get to work or get comfortable at home. Probably feels like you want to cut your leg off. |
| Week 2 | Starting to take the right pain killers, this helps a bit. Work is a killer, leg still extremely painful. |
| Week 4 | Starting to improve slightly after making appropriate lifestyle changes, optimising diet and using the specific exercises to my individual problem. |
| Week 6 | Feeling significantly better. Feeling like you can get through a day at work without too much pain in the evening. Still very wary of your back. |
| Week 9 | Leg is much better but back still stiff. Trying to get that last bit of movement back now. Terrified of the thought of swinging a golf club again. |
| Week 12 | Through practicing methods in order to regain normal function, you’re seeing an improvement in confidence. You feel ready to go back to the things you love but know you need to still be cautious for a while. |
Here is a video guide on how to ensure the healing process goes as quickly as possible:
With help recognising the signs of a healing herniated disc, check out the following article: Signs A Herniated Disc Is Healing (2023 Complete Guide).
#2 Spinal Stenosis
Stenosis refers to the narrowing of a body channel – in this case, the spinal canal. Age- and activity-related wear-and-tear of the spine can degenerate the spinal canal.
As the spinal canal narrows, it compresses against the spinal cord and pinches the nerve roots. Stenosis can be localised to one area or globalised throughout the entire spine. Globalisation of stenosis, meaning a widespread narrowing of the spinal canal experienced throughout the entire spine, is called “True Spinal Stenosis”. However, onset of spinal stenosis is most frequently witnessed in the lower back (the lumbar area) or the neck, given these areas are most frequently recruited for movement.
There are two primary processes which lead to spinal stenosis: degeneration of cartilage and the development of bone spurs. Spinal wear-and-tear erodes away the cartilage which buffers the spinal joints (the places where two vertebrae meet). Without this cartilage, the bones end up grinding against each other, closing the space around the nerves.
Another key process that occurs, which contributes to spinal stenosis, is the development of bone spurs (called osteophytes). When the joint is damaged, new bony growths can develop on the vertebrae. The bone growths themselves do not usually cause pain. However, these growths take up space which narrows the spinal canal. When bone spurs develop in the foramen (notably in the lumbar area) they can press against the sciatic nerve roots, causing pain along the sciatic nerve.
Pins and needles and/or numbness in the legs or feet are also common with stenosis induced sciatica. Spinal stenosis can cause sensory changes in the leg and/or foot, and for some people these “funny” sensations can be worse than the pain.
This symptom happens because the reduction of space in the spinal canal causes the surrounding structures to press against the nerve in the spine, stopping the nerve from doing its job correctly. This means that some signals don’t get through properly and sensation is distorted. For more information about pins and needles with sciatica, please read the following article.
How to treat it
Unfortunately, due to the degenerative nature of the structural and functional changes in the spine, spinal stenosis is irreversible. So, when I talk about treatment, I am referring to measures which can be taken to relieve some of the symptoms you are experiencing.
Exercise
Physical therapy is one of the most promising treatments for spinal stenosis. A proper rehabilitation program will help people with spinal stenosis by doing the following:
- Improving the flexibility of the muscles in the legs and reducing the “pull” on the spine so you can walk for further before pain
- Relieving tension in the back muscles and reducing back pain
- Improving fitness capacity so you walk for further with perfect technique, delaying pain
- Improving flexibility in the spine which lubricates the joints that the nerves run through
- Restoring health to the pinched nerves and reducing leg pain
I think the above constitutes a pretty compelling argument for having a good exercise program for spinal stenosis!
However, it’s very easy to get it wrong when selecting exercises for spinal stenosis. Please refer to this article of mine to see the spinal stenosis exercises you should avoid to avoid exacerbating your pain.
Now let’s look at some of the best exercises for spinal stenosis.
The common theme for the recommended exercises for spinal stenosis is that they all involve the opposite of spinal extension – we call this movement FLEXION.
Flexion exercises for spinal stenosis tend to bring about a much better outcome than extension exercises. Flexion exercises open up the narrowed spaces in the spine which allows the compressed nerves to “breathe” for a while, relieving symptoms effectively.
The following is a typical exercise program I might prescribe for someone with spinal stenosis. Bear in mind that what I find on my assessment dictates which exercises I might prescribe; some of these exercises may not be suitable for you. Always get an assessment from a healthcare professional before starting any new exercise programme.
The Program:
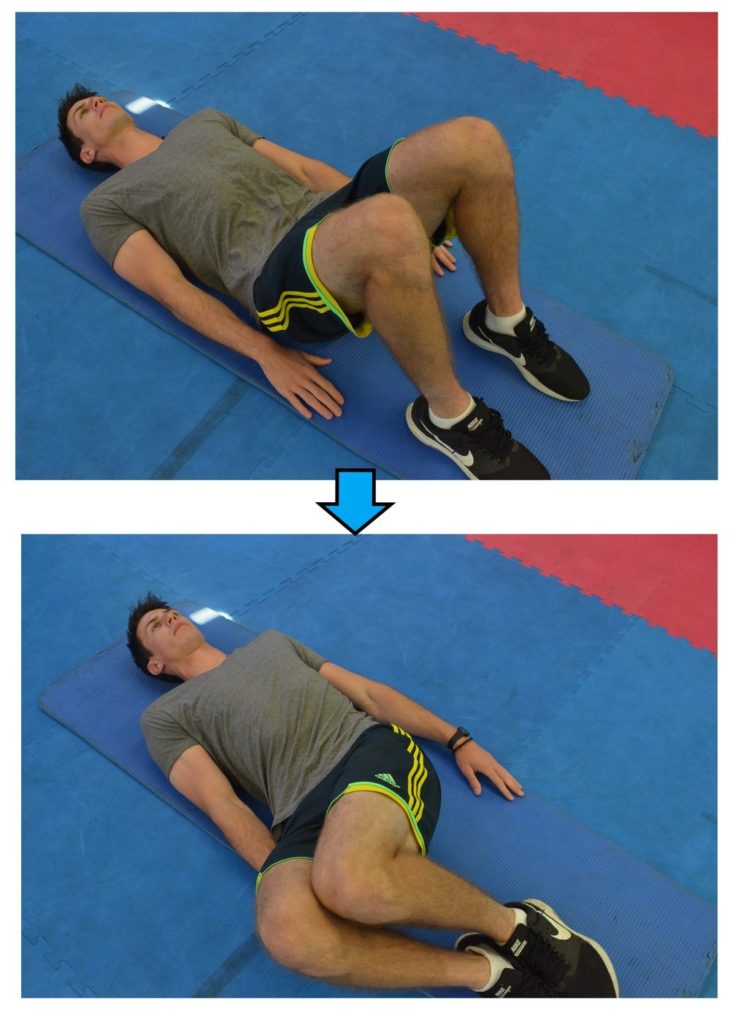
Knee Hugs: 10 repetitions on each side; morning, afternoon and evening

Gluteal Stretch: 30-second hold x 2 each side; morning and evening

Hip Flexor Stretch: 30-second hold x 3 each side; morning and evening
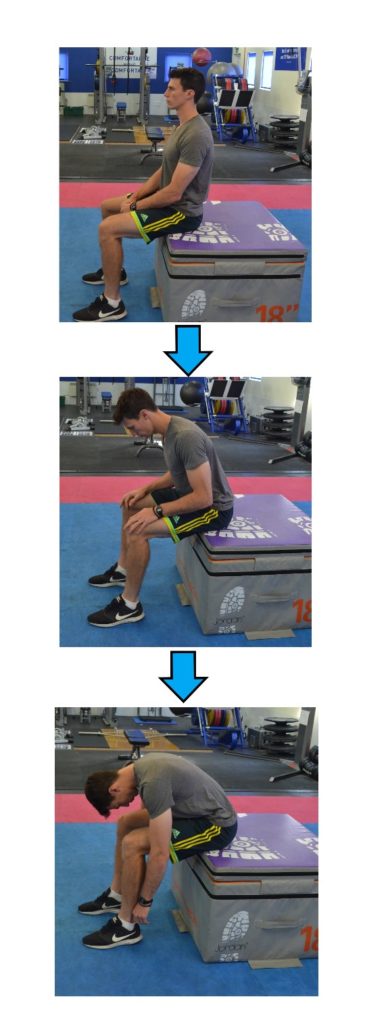
Flexion in Sitting: 5 slow repetitions; morning, afternoon, evening and whenever in pain
For a full article, with pictures and extended descriptions of each stretch and activity, please check out the following linked article.
Pharmaceutical and Surgical Intervention
There are a range of pharmaceutical options your medical specialist might offer to help relieve some of the pain or discomfort you are experiencing. The following are some interventions and their benefits:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): many NSAIDs are available over the counter, Ibuprofen being the most common. These medications provide pain relief by targeting inflammation which may be causing aches and adding pressure to your nerves. However, your medical specialist might prescribe some stronger or longer lasting NSAIDs, such as Naproxen.
- Anti-seizure drugs: often prescribed to help manage the pain resulting from nerve damage (gabapentin or pregabalin are examples of effective anti-seizure medications)
- Epidural Steroid Injection (ESI): offering powerful pain relief, found to be most helpful for the legs, ESIs are administered to the epidural space which surrounds the spinal nerves.
Alternatively, although we want to avoid surgery, sometimes it may be the only option for relief. There are surgical treatments which can help relieve symptoms:
- Laminotomy or laminectomy: there are 10 laminae in the spine. A lamina is a part of the bone surrounding the back of the spinal cord. Partial segments of a lamina can be removed to relieve pressure on the spinal nerves – this is called a laminotomy.
- In more extreme cases the entire lamina may be removed to increase the space around your spinal cord. This is known as a laminectomy (or decompression – which describes the reversal of the nerve compression).
#3 Piriformis Syndrome
This condition is conveniently named after the muscle which is responsible for the problem. The piriformis muscle is located in the buttocks; we have two piriformis muscles, one on each side, which run from the bottom of the spine to the top of the thigh. It’s an important muscle for the movement of your hips and your pelvis. If you are ever experiencing buttock pain which is isolated specifically to your gluteus and is causing numbness around this area it is likely caused by your Piriformis.
The sciatic nerve passes very closely underneath the piriformis muscle, as it travels through the buttock region.
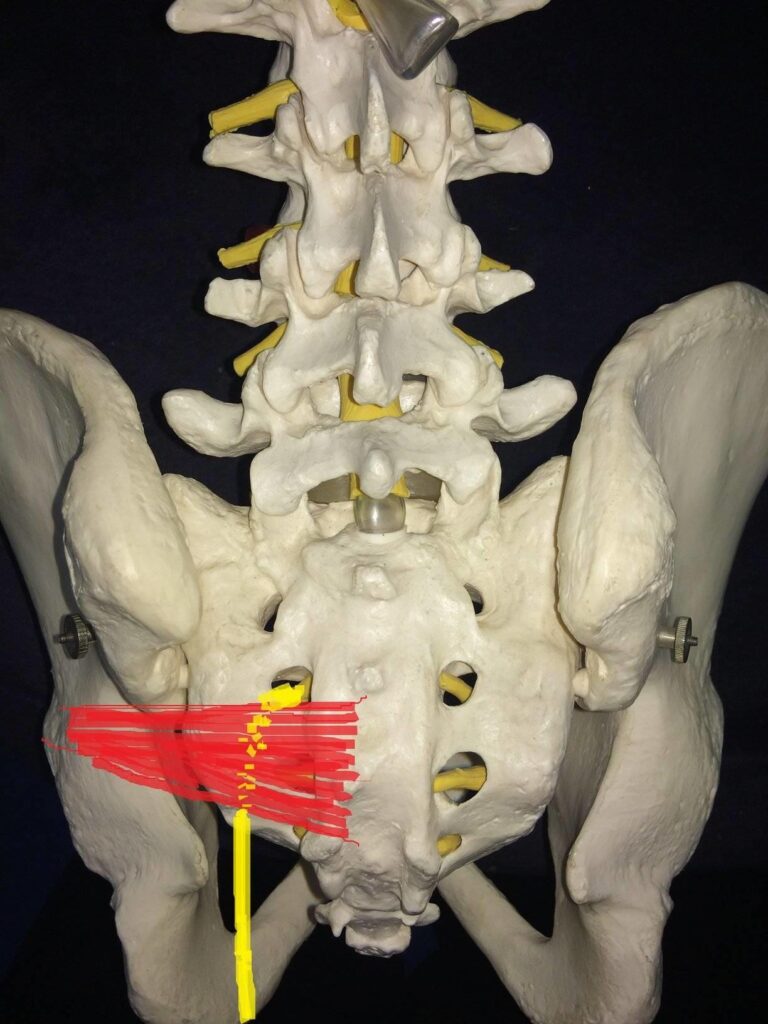
The left piriformis muscle is shown in red, with the yellow drawing depicting where the sciatic nerve runs.
Damage to the piriformis muscle can cause swelling, inflammation and/or muscle spasms, all of which can alter the shape of the muscle (a swelling muscle will increase in size). These changes to the muscle can force it to press against the sciatic nerve.
Some people think of sciatica and piriformis syndrome as the same thing; technically, sciatica describes the SYMPTOM, while piriformis syndrome can be the CAUSE of the symptom.
The onset of piriformis syndrome is usually traceable to an activity or injury from the last few days. Damage to the piriformis muscles is most likely to occur following strained or overly extensive activity. For example, exercising without properly warming up or repetitive activity for extended periods of time (such as running).
Don’t be fooled, however, inactivity can be equally damaging. For example, sitting still for too long (often witnessed in individuals working at their desk all day) can compress the piriformis muscle against your sciatic nerve. Sitting for long periods of the day can cause piriformis syndrome due to the weakening and lengthening of the gluteal muscles. When this occurs, the piriformis is made to work extra hard to compensate for the weakness in other areas, which can eventually lead to muscle spasms in the piriformis.
Additionally, those with tight muscles (caused by inactivity) are more likely to then pull a muscle when active again. It’s a bit of a catch-22!
How to treat it
Overall, if you want to avoid sciatica from piriformis syndrome, it’s important to establish a good balance when it comes to activity. Make sure you take regular breaks when sitting, always warm up before activity and try not to over exert yourself during exercise.
The great news is piriformis syndrome usually only takes a few days or weeks to heal. As with most muscle-based issues, rest is key. Allowing time for sweeling and/or spasms to reduce is the key to preventing irritation of the sciatic nerve by the piriformis muscle.
Additionally, if you are suffering from piriformis syndrome, there are several key stretches I recommend to relieve the pain. Find them described, with picture demonstrations, here.
Finally, for a more comprehensive layout of your treatment options, please visit my ultimate guide to treating you piriformis syndrome!
Mimicking Conditions
There are several conditions which can produce symptoms which mimic the symptoms of sciatica and make it difficult to type of sciatica you have, because you may not have sciatica at all! Let’s go over a few of the culprits.
Sacroiliac joint dysfunction:
The sacroiliac joint is depicted below.
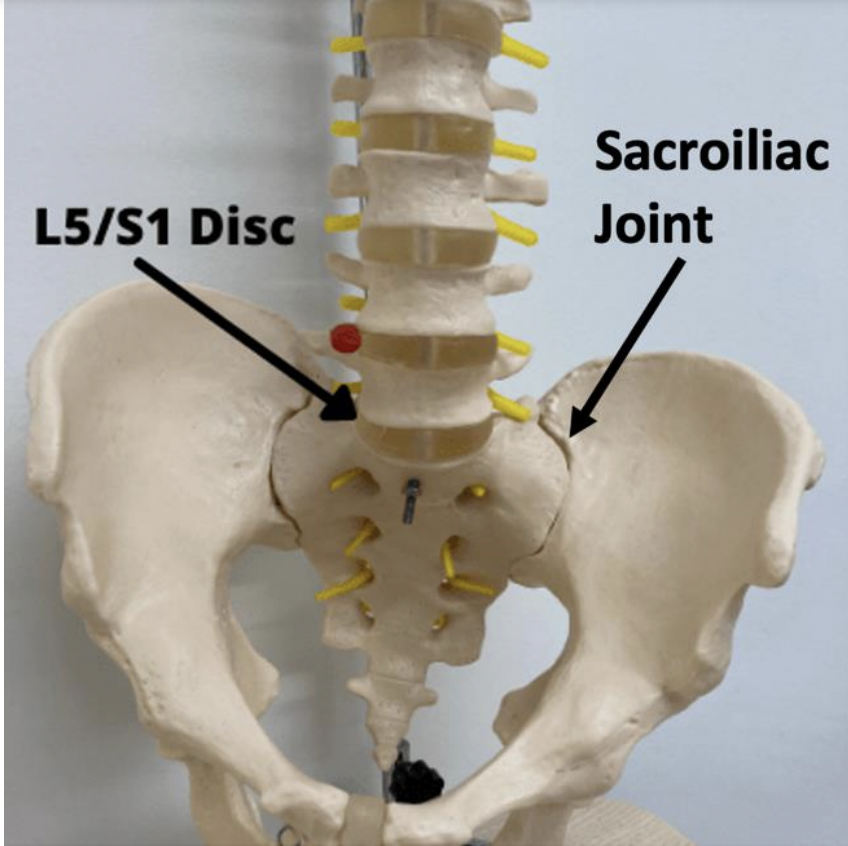
When improper movement, too much or too little, occurs at this junction, it can lead to dysfunction and pain. Pain radiates down the leg in the same manner witnessed with a lumbar disc herniation, making the two conditions difficult to differentiate. Treatment focuses of rehabilitating the joint, the restore regular movement.
Peripheral neuropathy:
Poor blood circulation, leading to nerve damage, is the primary cause of peripheral neuropathy. The symptoms differ from sciatica, in that the pain often starts in the toes or feet, before traveling UP the leg. This pain is commonly experienced in both legs, rather than just one which is usually the case for sciatica. Without treating the underlying cause of peripheral neuropathy, you open yourself up to a whole wealth of other problems, such as infections which result in limb amputations.
Peroneal neuropathy:
Peroneal neuropathy is a form of peripheral neuropathy. The peroneal nerve branches off from the sciatic nerve, supplying sensation to front of the legs and top of the feet, as well as controlling muscular movement in the ankle and toes. Injuries to your knee(s) can damage the peroneal nerve which can cause pain and/or affect movement in the feet. Although the symptoms may mimic sciatica, the treatment will focus on supporting the knee and/or leg, rather than the spine.
Here is a video about peroneal neuropathy, including the location of the pain and how to treat it:
Overall top tip – Improving Your General Health
As we’ve covered, there are many different conditions which can result in sciatica; even some problems that mimic sciatica. However, as we’ve stated when discussing treatment options, it is important to identifying what type of sciatica you have.
If you’re struggling with pain or mobility restriction, one thing that might help is to address other general health issues like your weight, your diet, and your general exercise.
If you’d like some tips on how to improve all of these aspects of your health, stave off injury and treat problems like sciatica and arthritis, you can grab a copy of my brand-new book, Thriving Beyond Fifty. You can see more details below:
Top Tip: Grab a copy of my #1 Best-Selling book, Thriving Beyond Fifty for more health, wellness and recovery strategies!
Click HERE to view the book on Amazon (UK)!
Click HERE to view the book on Amazon (USA)!
Summary
I hope this article has helped you to answer the question “Which Type of Sciatica Do I Have?”
As you can see, there are many different “types” of sciatica, with each type causing somewhat similar symptoms with subtle differences. As previously mentioned, it is always wise to seek a professional assessment from a doctor or physio who can give you a better idea as to which type of sciatica you have.
Did you gain something from this article? Leave a comment below!
The information in this article is provided for informational purposes and should not be used as a substitute for medical advice. Seek a medical assessment for any new or existing case of sciatica.

