One of the most common questions I get asked is “how is it possible to have sciatica without back pain?” Well, this article is here to answer that question for you!
Sciatica without back pain is a common complaint – and while it can seem confusing, there is usually a sensible answer to why someone might be suffering from sciatica without back pain.
The first step in understanding sciatica without back pain is to understand the anatomy of the spine and the sciatic nerve.
Sciatica Without Back Pain: Basic Anatomy
Firstly, let’s go over some of our basic anatomical structures to explain why this happens:
The spine is made up of 24 movable bones called vertebrae. Each of these bones are separated by an intervertebral disc – a tough sac made of strong cartilage, filled with fluid. The outer layer is called the annulus fibrosus, which holds a jelly-like centre called the nucleus pulposus. These discs act as cushions to absorb the impact of movement and prevent the vertebrae from grinding against each other.
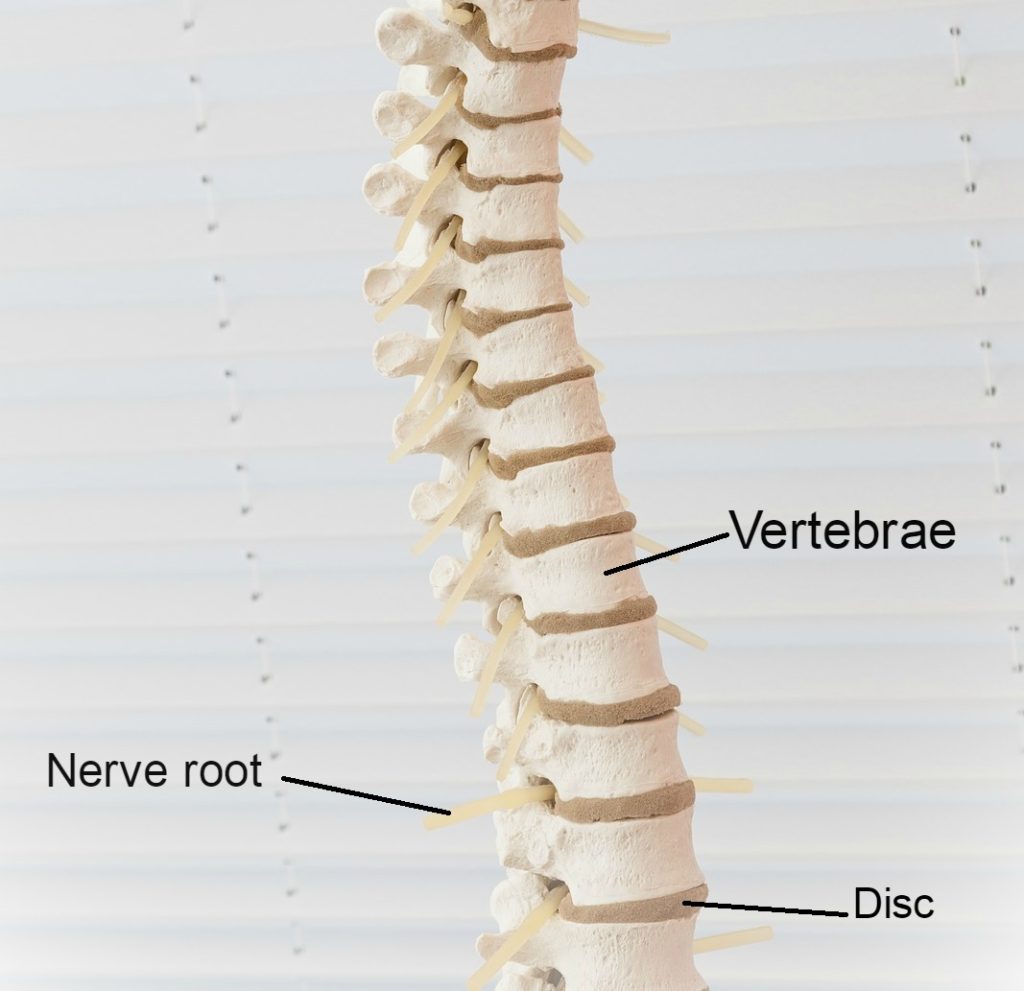
The spine not only functions to provide structure for our body, offering support for the body to complete movement, but it is also responsible for housing the spinal cord. This “house” is called the spinal canal – a tunnel through the spine whereby the spinal cord runs. The spinal cord runs from your brain all the way down to the bottom of your back, supplying nerves throughout your entire body.
Your lower back, called the lumbar spine, is made up of 5 large lumbar vertebrae. These are called L1 to L5; with L5 being the lowest vertebra in the spine. We name these discs based on the vertebrae above and below the disc. For example, if we are talking about the disc between L4 and L5, we would call it disc L4/L5.
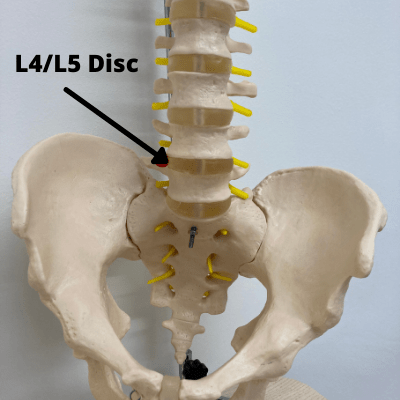
Our lumbar spine supplies the nerves to our legs. Injury or wear and tear to this area is common, given our lumbar area is one of our most frequently recruited sites for movement. Because of the way our spines are designed, they have special curves at the top, middle and bottom. When we walk and move, the areas that have a more dramatic curve tend to suffer from more stress than the areas that don’t curve. The lumbar spine has one of such curves, which is why problems often occur in this area.
Sciatic Nerve Anatomy
Your sciatic nerve is the largest in the body, running from your lower back and down through your legs. Compression or irritation of the sciatic nerve roots can cause the pain known as sciatica – typically a sharp, shooting pain that may prevent you from being able to perform much movement. Sciatica is not a “disease” in and of itself. “Sciatica” simply describes a set of symptoms that can be caused by a number of conditions.
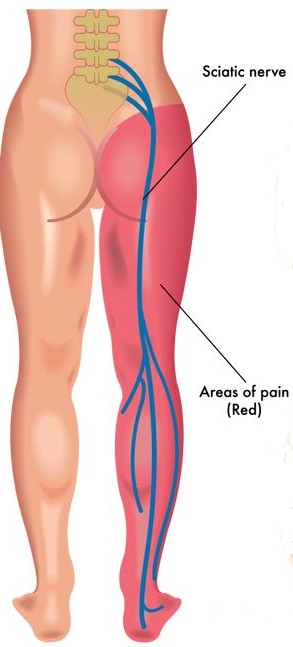
Because of the length of the sciatic nerve, the pain may run from your back into your buttock and all the way down one leg. Because your sciatic nerve is responsible for sending messages and relaying feeling down your legs, issues with the spine often cause pain, aching or distorted sensation along this pathway, rather than at the nerve root itself. For this reason, sciatica without back pain can occur, even if the injury is located in the back.
Conditions that can cause sciatica without back pain
Now, let’s have a look at some of the most common conditions which can cause sciatica without back pain. Despite these conditions often stemming from problems in the spine, back pain isn’t always present. Let’s explore why.
Lumbar Spondylosis
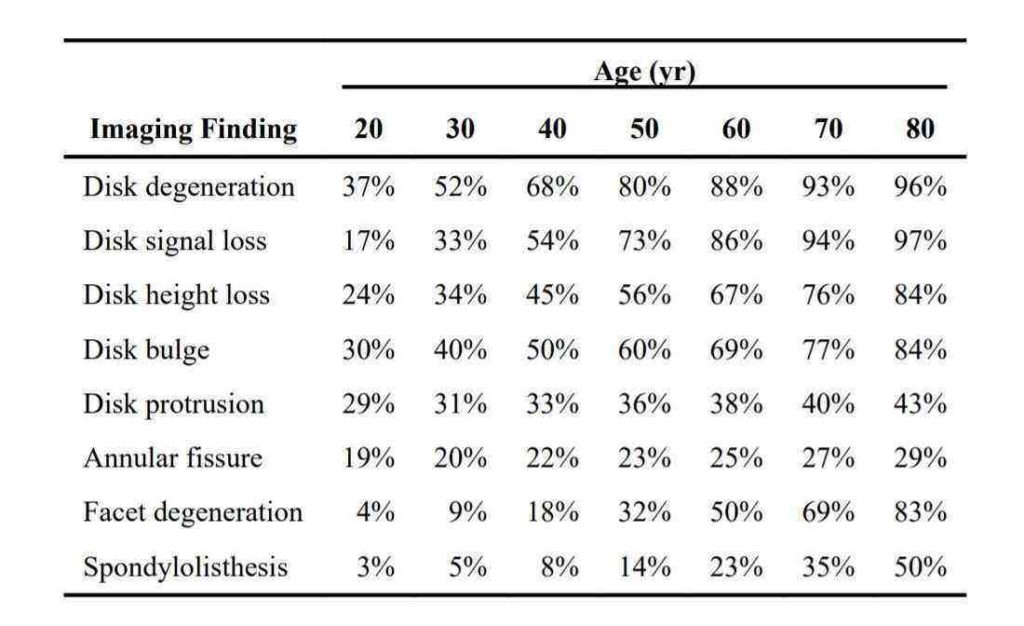
Another label for lumbar spondylosis is disc degeneration disease, which offers insight into the root of the problem. Spondylosis is a descriptive term, representing an umbrella of different spinal conditions which occur as the result of age-related spinal degeneration.
Ageing is the predominant catalyst for spinal spondylosis. The impact of everyday activity accumulates as we age, leading to spinal “wear and tear”. After the age of 40, most people experience some degree of disk degeneration; not everyone experiencing degeneration also experiences pain. For individuals aged over 60, lumbar spondylosis was present in over 75%. However, only just over 25% suffered from lower back pain.
Ageing in and of itself is not the root cause of spinal spondylosis. Instead, ageing is often associated with the development of arthritis – a condition whereby inflammation and/or degeneration is observed at the joints (the areas where two bones meet).
In this case, age-related degeneration is witnessed in the lumbar discs. With time, the spinal discs dehydrate and shrink, losing their lubrication. When discs significantly dehydrate, they may crack which can cause a herniated disc (we will explore this more later)! Without these cushioning structures, the vertebrae are left to grind against each other, often making our movements stiff as they lack the substance which help the joints glide.
So, how does this cause sciatica?
Arthritis-induced inflammation at the lower back joints can put pressure on the sciatic nerve roots, sending pain down the nerve channel. Additionally, disc degeneration equates to a smaller space for the nerves in the spine, causing them to become compressed.
Interestingly, this condition can cause sciatica without back pain, even though the damage and injury occurs in the back. We do not fully understand why some people do have back pain while others have sciatica without back pain with this condition, but it might be due to the way the brain and the nerves process the pain information coming from the site of the injury.
When this compression becomes more severe, it leads to a condition called “spinal stenosis” which is a key cause of sciatica.
Spinal Stenosis
Spinal stenosis falls under the umbrella of spondylosis, with similar degenerative features responsible for the problem. Stenosis refers to the narrowing of a body channel – in this case, the spinal canal. Age- and activity-related wear-and-tear of the spine can degenerate the spinal canal.
As the spinal canal narrows, it compresses against the spinal cord and pinches the nerve roots. This is highly painful as nerves are incredibly sensitive. Stenosis can be localised to one area or globalised throughout the entire spine. Globalisation of stenosis, meaning a widespread narrowing of the spinal canal experienced throughout the entire spine, is called “True Spinal Stenosis”. However, onset of spinal stenosis is most frequently witnessed in the lower back (the lumbar area) or the neck, given these areas are most frequently recruited for movement.
There are two primary processes which lead to spinal stenosis: degeneration of cartilage and the development of bone spurs. Spinal wear-and-tear erodes away the cartilage which buffers the spinal joints (the places where two vertebrae meet). Without this cartilage, the bones end up grinding against each other, closing the space around the nerves.
Another key process that occurs, which contributes to spinal stenosis, is the development of bone spurs (called osteophytes). When the joint is damaged, new bony growths can develop on the vertebrae. The bone growths themselves do not usually cause pain. However, these growths take up space which leads to the narrowing of the spinal canal.
The areas where the nerve root exits the spine is called the foramen. When bone spurs develop in this area (notably the foramen in the lumbar area) they can press against the sciatic nerve roots, causing pain along the sciatic nerve.
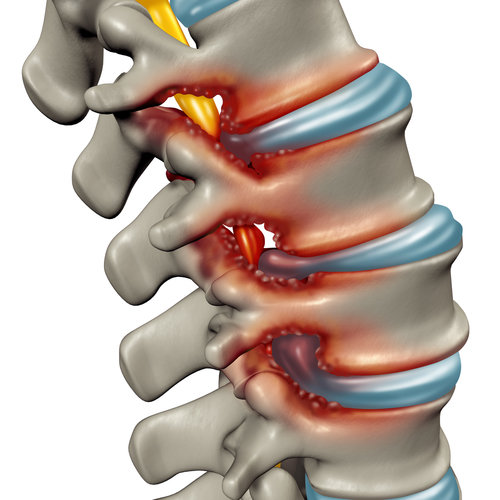
The red “bumps” in the above image demonstrate bone spurs which reduce the space around the nerves.
With stenosis induced sciatica, pins and needles and/or numbness in the legs or feet are also common. Spinal stenosis can cause sensory changes in the leg and/or foot. Usually, the funny sensations will be present in the foot and toes and for some people this symptom can be worse than the pain. This symptom happens because the reduction of space in the spinal canal causes the surrounding structures to press against the nerve in the spine, stopping the nerve from doing its job correctly. This means that some signals don’t get through properly and sensation is distorted.
Spinal stenosis often causes back pain, but spinal stenosis can also cause sciatica without back pain. Commonly, the symptoms can be felt in just the backs of the calves when walking. Sometimes, back pain happens at the same time but quite often there is no back pain.

Spinal stenosis can also cause pins and needles. For more information about pins and needles with sciatica, please read the following article.
Disc Bulge or Disc Herniation
A disc bulge is when one or more disc bulges outwards from its usual place in between two vertebrae. When the disc protrudes outwards, it can press against the spinal nerve roots (as shown in the picture below).

The above picture shows a bulging disc pressing against the nerve root (the yellow stem) as it exits the foramen.
Touching, pinching, or compressing a nerve causes reactions around that area, causing pain along the entire course of the nerve. You will get sciatica symptoms from the direct contact but also a chemical reaction around that area which exacerbates these symptoms. The chemical reaction that occurs when we compress a nerve, especially when part of a spinal disc touches the sciatic nerve, is similar to the type of reaction we get when we are stung by a bee.
If one part of the disc has weakened significantly more than others, it can lead to something called a herniated disc. This describes the event whereby the strong outer fibres of the disc split (or “herniate”) and the fluid within the disc leaks out at the region where the injury occurred. This is different from a bulging disc, whereby the outer layer remains intact enough to contain the centre (nucleus pulposus).
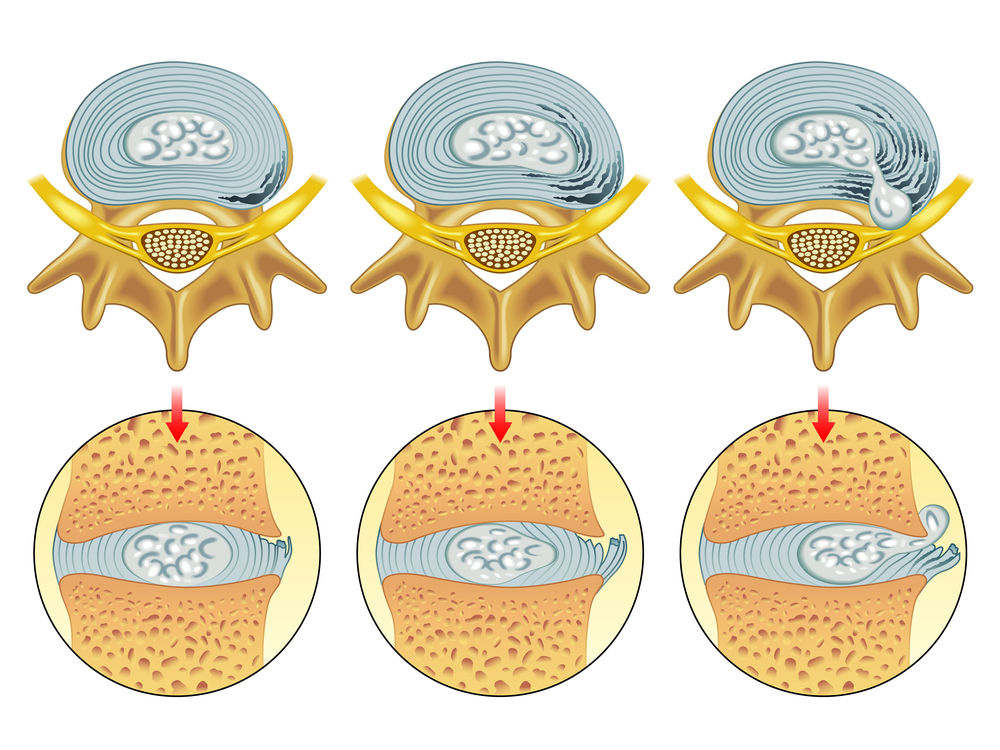
The above shows different degrees of disc damage. The left-hand and middle image show bulging discs, whilst the right-hand image shows a herniated disc.
A herniated disc is more likely than a bulging disc to cause sciatica, as the disc protrudes further, making it more likely to affect the surrounding nerve roots. A herniated disc is an extremely common problem. So common, in fact, that 1 in 10 people will suffer from sciatica at some point in their lives and the vast majority of those cases are caused by a herniated disc.
If someone suffers from a herniated disc at L5/S1, a disc which is extremely close in proximity to the sciatic nerve, the inner material from the disc often touches the nerve and can cause L5/S1 nerve root compression symptoms, which include sciatica, numbness and weakness in the leg.
A herniated disc or bulging disc can cause sciatica without back pain. There are no nerves directly within the discs, so a disc injury does not directly cause back pain in the region of the injury. The back pain that usually occurs with a bulging or herniated disc is usually associated with a muscle spasm caused by a “shock” reaction in the back. Sometimes, the muscular spasm that leads to back pain with a herniated or bulging disc never happens, so there can be sciatica without back pain.
For information about how to treat a herniated disc, please visit the following article.
Piriformis Syndrome
This condition is conveniently named after the muscle which is responsible for the problem. The piriformis muscle is located in the buttocks; we have two piriformis muscles, one on each side, which run from the bottom of the spine to the top of the thigh. It’s an important muscle for the movement of your hips and your pelvis. If you are ever experiencing buttock pain which is isolated specifically to your gluteus and is causing numbness around this area it could be caused by your Piriformis.
The sciatic nerve passes very closely underneath the piriformis muscle, as it travels through the buttock region. Usually, this occurs without any problems but in some people (due to an anatomical variation) the sciatic nerve can travel directly through the piriformis muscle. The hypothesis is that it is these people who are in danger of developing priiformis syndrome.
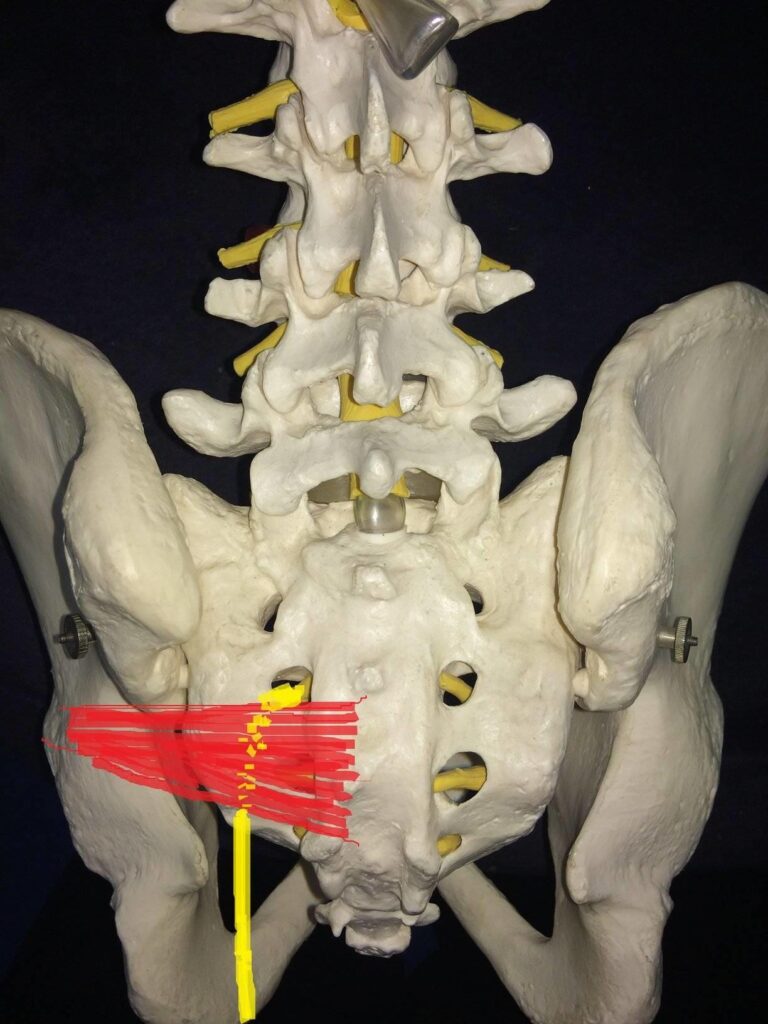
The left piriformis muscle is shown in red, with the yellow drawing depicting where the sciatic nerve runs.
Issues with the piriformis muscle can cause swelling, inflammation and/or muscle spasms, all of which can alter the shape of the muscle (a swelling muscle will increase in size). These changes to the muscle can force it to press against the sciatic nerve.
If there is a problem with the piriformis impinging the sciatic nerve, sciatica without back pain can occur. This is because the piriformis is not within the back. People with piriformis syndrome often have buttock pain with sciatica, but no back pain.
Issues with the piriformis muscle is most likely to occur following strained or overly extensive activity. For example, exercising without properly warming up or repetitive activity for extended periods of time (such as running).
Don’t be fooled, however, inactivity can be equally damaging. For example, sitting still for too long (often witnessed in individuals working at their desk all day) can compress the piriformis muscle against your sciatic nerve. Additionally, those with tight muscles (caused by inactivity) are more likely to then pull a muscle when active again. It’s a bit of a catch-22!
Overall, if you want to avoid sciatica, it’s important to establish a good balance when it comes to activity. Make sure you take regular breaks when sitting, always warm up before activity and try not to over exert yourself during exercise.
For more information about piriformis syndrome including how it is diagnosed, treated and prevented, please refer to the following article.
Summary of Sciatica Without Back Pain
In this article we’ve looked at some of the most common spinal conditions which cause sciatica without back pain. Although these conditions relate to changes in the spine and sciatic nerve, they don’t always cause back pain. Rather, the spinal changes can impact the sciatic nerve, which causes pain to the lower body. The side of your body through which the pain radiates (left or right) will usually indicate which sciatic nerve is compromised.
Nerve compression can be extremely painful, and if left untreated can cause permanent damage. If you experience weakness in the legs (particularly calf and foot weakness with a L5/S1 nerve root compression), this indicates a severe nerve compression. If this sounds like you, it needs addressing as soon as possible. Please contact a medical professional ASAP – don’t leave it until it’s too late!
References
1. Muraki, S., Oka, H., Akune, T., Mabuchi, A., En-yo, Y., Yoshida, M., Saika, A., Suzuki, T., Yoshida, H., Ishibashi, H. and Yamamoto, S., 2009. Prevalence of radiographic lumbar spondylosis and its association with low back pain in elderly subjects of population-based cohorts: the ROAD study. Annals of the Rheumatic Disease

