Simply put: sciatica happens when compression or irritation occurs at the sciatic nerve.
Although this explanation for why sciatica happens may sound fairly simple, I advise not closing this article too hastily. Exactly how and why this compression or irritation of the sciatic nerve occurs is a far more complex issue which needs exploring.
This article aims to do the following:
- Describe what sciatica is
- Detail the 6 leading conditions which can cause sciatica
- Outline some of the contributing risk factors for the onset of sciatica
- Offer advise for avoiding and/or treating sciatica
Let’s kick off by going over some of our most important anatomical structures, to make sure we understand how they are involved in sciatica.
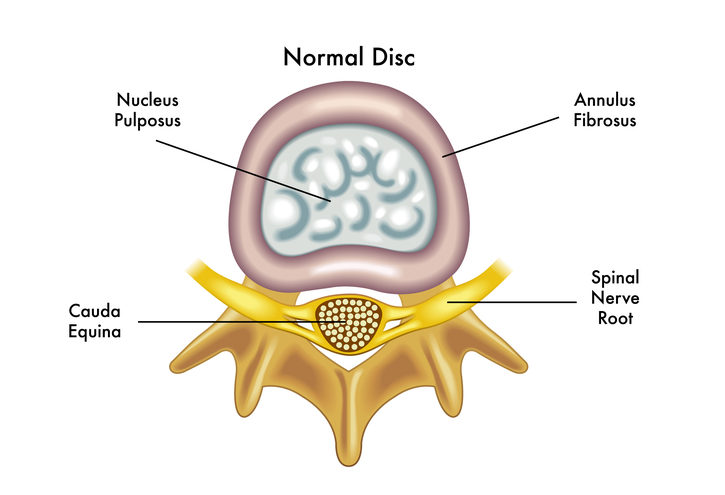
The spine is made up of 24 movable bones called vertebrae. Each of these bones are separated by an intervertebral disc – a tough sac made of strong cartilage, filled with fluid. The outer layer is called the annulus fibrosus, which holds a jelly-like centre called the nucleus pulposus. These discs act as cushions to absorb the impact of movement and prevent the vertebrae from grinding against each other.
The spine not only functions to provide structure for our body, offering support for the body to complete movement, but it is also responsible for housing the spinal cord.
This “house” is called the spinal canal – a tunnel through the spine whereby the spinal cord runs. The spinal cord runs from your brain all the way down to the bottom of your back, supplying nerves throughout your entire body.
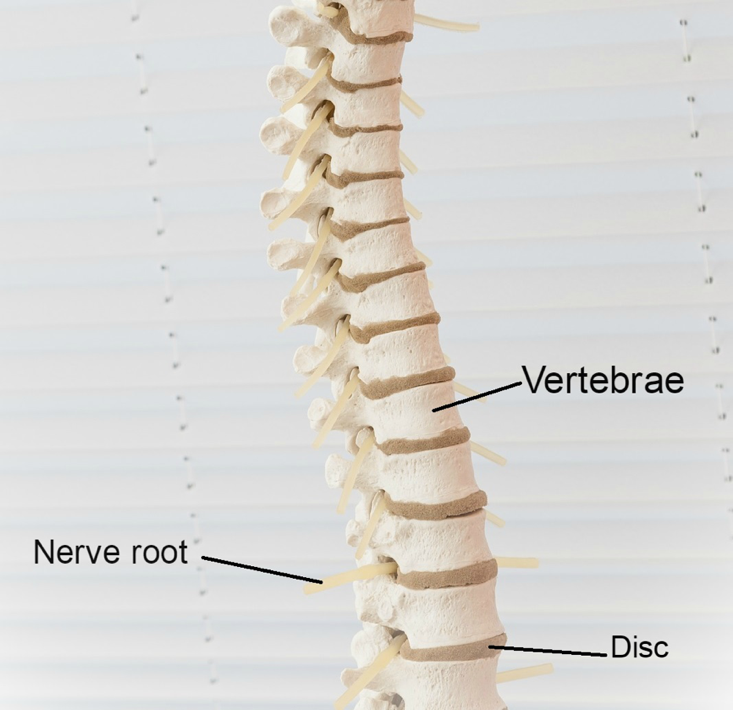
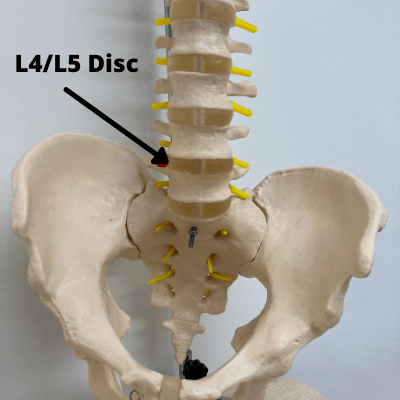
Your lower back, called the lumbar spine, is made up of 5 large lumbar vertebrae. These are called L1 to L5; with L5 being the lowest vertebra in the spine. We name these discs based on the vertebrae above and below the disc. For example, if we are talking about the disc between L4 and L5, we would call it disc L4/L5.
Our lumbar spine supplies the nerves to our legs. Damage to this area is common, given our lumbar area is one of our most frequently recruited sites for movement. Because of the way our spines are designed, they have special curves at the top, middle and bottom.
When we walk and move, the areas that have a more dramatic curve tend to suffer from more stress than the areas that have less of a curve. The lower lumbar spine (L4-S1) has the most dramatic curve in the spine, making this region (compromising of L4, L5 and S1) the most likely to suffer injury. This is also the region that contains the nerves that make up the sciatic nerve.
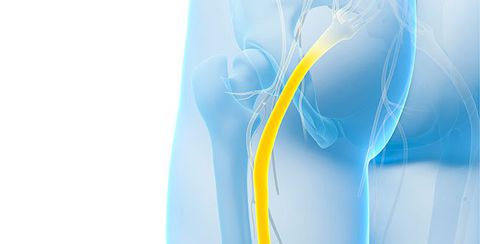
Your sciatic nerve is the largest in the body, running from your lower back and down through your legs. Compression or irritation of the sciatic nerve roots can cause the pain known as sciatica – typically a sharp, shooting pain that may prevent you from being able to perform much movement.
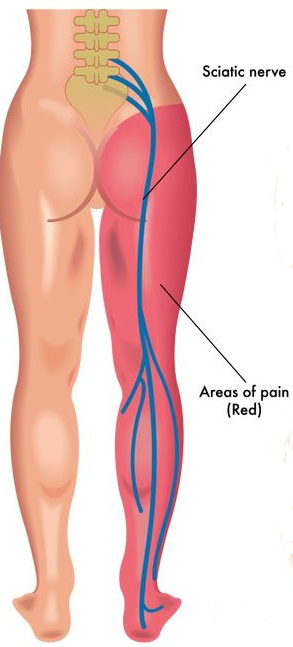
Because of the length of the sciatic nerve, the pain may run from your back into your buttock and all the way down one leg. Because your sciatic nerve is responsible for sending messages and relaying feeling down your legs, issues with the spine often cause pain, aching or distorted sensation along this pathway, rather than at the nerve root.
Here is a full list of the sciatica symptoms one can expect with this condition.
Now let’s go over some of the most common conditions which I see when treating patients for sciatica.
Why Sciatica Happens: The 6 Most Common Causes:
#1 Disc Bulge or Herniation
A disc bulge is when one or more of the discs bulge outwards from their usual place in between two vertebrae. This happens due to a weakness in the annulus fibrosis (outer layer of the disc) that worsens over time. The inner material (called the nucleus pulposis) can then “bulge” towards the back part of the disc, causing a protusion.
When the disc protrudes outwards, it can press against the spinal nerve roots, that also exist at the back of the spine.

The above picture shows a bulging disc pressing against the nerve root (the yellow stem) as it exits the spine (this gap is called the foramen).
Touching, pinching, or compressing a nerve causes reactions around that area, causing pain along the entire course of the nerve. You will get sciatica symptoms from the direct contact of the disc on the nerve – but also a chemical reaction around that area which exacerbates these symptoms.
The chemical reaction that occurs when we compress a nerve, especially when part of a spinal disc touches the sciatic nerve, is similar to what we get when we are stung by a bee. We now know that it is the inflammatory chemicals in this area that cause a lot of the pain experienced in sciatica, as opposed to just the direct pressure of the disc on the nerve.
If one part of the disc has weakened significantly more than others, it can lead to a herniated disc. This describes the event whereby the strong outer fibres of the disc split (or “herniate”) and the fluid within the disc actually leaks out at the region where the injury occurred. This is different from a bulging disc, whereby the outer layer remains intact enough to contain the centre (nucleus pulposus).
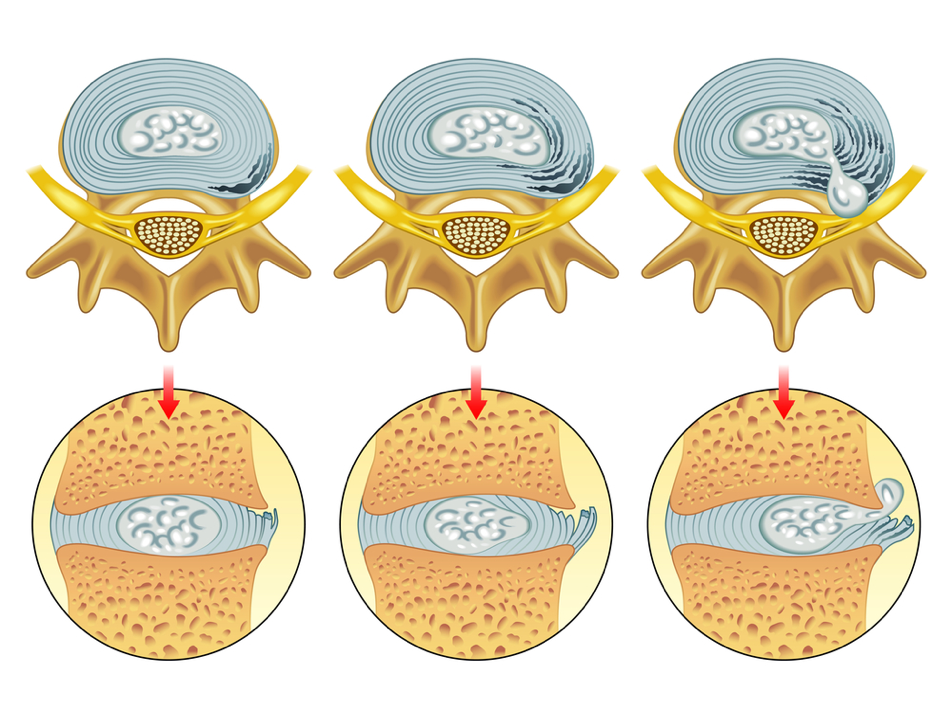
The above shows different degrees of disc damage. The left-hand and middle image show bulging discs, whilst the right-hand image shows a herniated disc.
A herniated disc is more likely than a bulging disc to cause sciatica, as the disc protrudes further, making it more likely to affect the surrounding nerve roots. However, the severity of the injury does not necessarily reflect the severity of the symptoms.
Some people with a bulging disc actually have worse symptoms than people with a herniated disc. We do not understand the reason why this happens. There is a lot of individual variation in terms of symptoms suffered by people with bulging or herniated discs.
A herniated disc is an extremely common problem. So common, in fact, that 1 in 10 people will suffer from sciatica at some point in their lives and the vast majority of those cases are caused by a herniated disc.
If someone suffers from a herniated disc at L5/S1 (where the lumbar spine and sacrum meet), a disc which is extremely close in proximity to one of the nerve roots that becomes the sciatic nerve, the inner material from the disc often touches the nerve root and can cause symptoms along the course of this nerve: which include sciatica, numbness, and weakness in the leg.
A herniated L5/S1 disc is one of the most common injuries I see when treating sciatica and is one of the most common reasons for why sciatica happens.
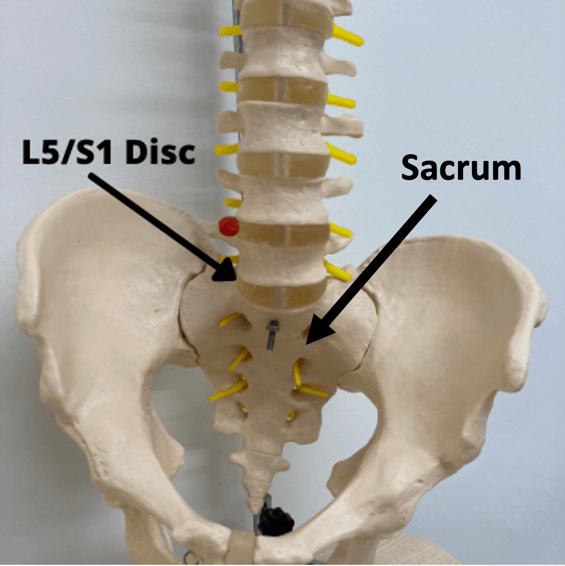
With an injury at L5-S1, there is often a typical L5 or S1 pain pattern. The pattern will depend on whether the L5 nerve root is affected, or whether the S1 nerve root is affected, or both.
The L5 pain pattern involves pain running down the OUTSIDE of the leg to the outer shin and then running to the outside border of the foot.
The S1 pain pattern is more like “classic sciatica” with pain running directly down the back of the leg, often all the way into the toes.
#2 Spinal Stenosis
Stenosis is a Latin term that refers to the narrowing of a bodily channel – in this case, the spinal canal. Age- and activity-related wear-and-tear of the spine can degenerate the spinal canal, causing the spaces that house the nerves to narrow severely. As the spinal canal narrows, it compresses against the spinal cord and pinches the nerve roots.
Stenosis can be localised to one area or globalised throughout the entire spine. A widespread narrowing of the spinal canal experienced throughout the entire spine, is called “True Spinal Stenosis”. However, onset of spinal stenosis is most frequently witnessed in the lower back (the lumbar area) or the neck, given these areas are most frequently recruited for movement.
There are three primary processes which lead to spinal stenosis: degeneration of cartilage, degeneration of the discs and the development of bone spurs.
Spinal wear-and-tear erodes away the cartilage which buffers the spinal joints (the places where two vertebrae meet). Without this cartilage, the bones end up grinding against each other, closing the space around the nerves.
Disc degeneration is a similar process, whereby the intervertebral discs that sit between the vertebrae lose their water content and become flatter than they otherwise would have been. This can also reduce the space in which the nerves exist.
Another key process that occurs which contributes to spinal stenosis is the development of bone spurs (called osteophytes). When the joint is degenerating, new bony growths can develop on the vertebrae. The bone growths themselves do not usually cause pain. However, these growths take up space which narrows the spinal canal. When bone spurs develop in the foramen (notably in the lumbar area) they can press against the sciatic nerve roots, causing pain along the sciatic nerve.
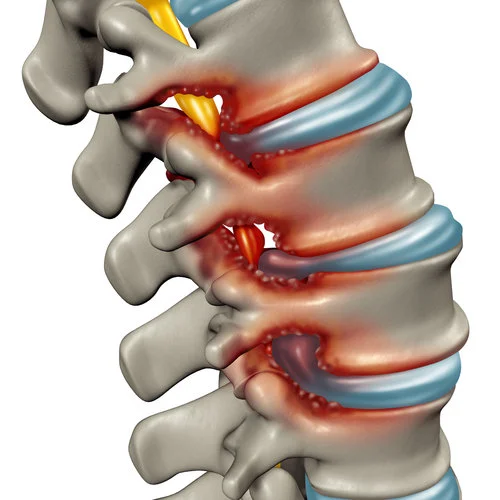
The red “bumps” in the above image demonstrate bone spurs which reduce the space around the nerves.
Get more information about spinal stenosis, including symptoms and treatment, here.
#3 Piriformis syndrome
This condition is conveniently named after the muscle which is responsible for the problem. The piriformis muscle is located in the buttocks; we have two piriformis muscles, one on each side, which run from the bottom of the spine (sacrum) to the top of the thigh bone (femur).
The piriformis is an important muscle for the movement of your hips and your pelvis. If you are ever experiencing buttock pain which is isolated specifically to your gluteus and is causing numbness around this area it could be caused by your piriformis.
The sciatic nerve passes very closely underneath the piriformis muscle, as it travels through the buttock region.
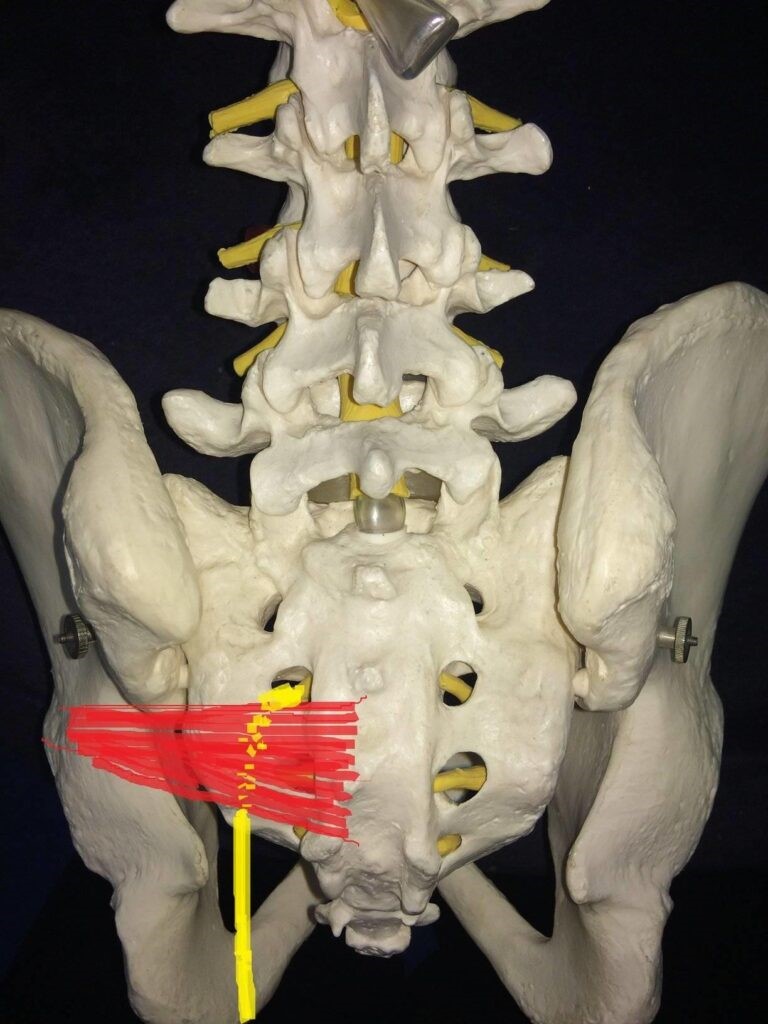
The left piriformis muscle is shown in red, with the yellow drawing depicting where the sciatic nerve runs.
Damage to the piriformis muscle can cause swelling, inflammation and/or muscle spasms, all of which can alter the shape of the muscle (a swelling muscle will increase in size). These changes to the muscle can force it to press against the sciatic nerve.
Some people think of sciatica and piriformis syndrome as the same thing; technically, sciatica describes the SYMPTOM, while piriformis syndrome can be the CAUSE of the symptom. You can read about the differences between “true” sciatica and piriformis syndrome in this article here.
The onset of piriformis syndrome is usually traceable to an activity or injury from the last few days or months. Problems with the piriformis muscle are most likely to occur following strained or overly extensive activity of the piriformis. The piriformis is only a small muscle and is often recruited to do jobs it was not designed to do when the other larger muscles are weak or “disconnected”.
The classic example that leads to piriformis syndrome is weakness in the gluteus medius muscle, causing the piriformis to become overworked when this muscle is underworking. The video below explains this phenomenon in more detail:
Inactivity can equally be a cause of piriformis syndrome. For example, sitting still for too long (often witnessed in individuals working at their desk all day) can compress the piriformis muscle against your sciatic nerve. Sitting for long periods of the day can cause piriformis syndrome due to the weakening and lengthening of the gluteal muscles.
When this occurs, the piriformis is made to work extra hard to compensate for the weakness in other areas, which can eventually lead to muscle spasms in the piriformis. Additionally, those with tight muscles (caused by inactivity) are more likely to then pull a muscle when active again.
You can read about piriformis syndrome in more detail with our ultimate guide here.
#4 – Injury to the Spine
A traumatic injury to the spine can sometimes cause sciatica either directly or indirectly.
In direct cases, trauma to the backside or lower back can cause inflammation around the nerve roots and lead to referred pain down the leg.
In indirect cases, a spinal fracture, spondylolisthesis or contusion can cause a nerve root to become pinched and lead to sciatica.
In any case of trauma to the spine, a thorough medical examination should be sought.
#5 – Tumours & Other Lesions
A spinal tumour (either benign or cancerous) can lead to impingement on the nerve roots in the spine or pelvis, depending on the site and size of the tumour. Tumours causing sciatica are thankfully rarer than the other causes of sciatica in this article.
These problems tend to start insidiously and can progress quickly or slowly. They tend to arise with a host of other symptoms, especially if the tumour is cancerous, such as weight loss, lumps, general feelings of malaise and night sweats. Sciatica due to a tumour tends to follow a “non-mechanical pattern”, where pain is not directly related to certain movements.
A medical practitioner would perform some tests and imaging to discern whether or not a tumour is the likely cause of sciatica.
#6 – Unexplained
Sometimes, sciatica can be present with no obvious cause, despite MRI scans and other investigations.
We would call this “idiopathic” sciatica, meaning sciatica with an unknown cause. This type of sciatica is common and can be frustrating to treat. There is some debate in the literature as to whether the cause in these instances is down to a problem with the way the brain processes pain, or a physical issue that cannot be seen on scans.
Despite there being no obvious cause, this type of sciatica can still do well with physiotherapy treatment and other treatment methods designed to help sciatica. We help people with this type of sciatica very often at my practice.
Speaking of excellent physical therapy programmes for most of the major causes of sciatica, my good friend, colleague and fellow international sciatica expert, Dean Volk, has a brand new sciatica relief video course available – and I’m delighted to be an official sponsor!

Check out Dean Volk’s “Kicking Sciatica OUT of the Butt!” Online Pain Relief Course Here!
I can proudly recommend Dean and his course for sciatica sufferers – because I’ve seen his incredible results first-hand. You can check out his course (and get lifetime access to the videos and bonus content) by clicking HERE.
General Risk Factors for Sciatica
Now that we’ve covered the most common conditions which cause sciatica, let’s have a look at some of the more general risk factors for sciatica.
#1 – Ageing
Ageing in and of itself is not the root cause of sciatica. Instead, ageing is often associated with the development of osteoarthritis, a form of arthritis conveniently labelled “wear and tear arthritis”.
Arthritis is a condition whereby inflammation and/or degeneration is observed at the joints (the areas where two bones meet). The structural and functional deterioration witnessed at the spinal joints can cause compression or irritation of the sciatic nerve roots.
Osteoarthritis is the most common cause of spinal stenosis; remember, they’re both labelled spinal wear-and-tear conditions. Roughly 80% of individuals over 55 years old demonstrate evidence of osteoarthritis. Wear and tear, and gradual bodily deterioration, is unavoidable. However, only 60% report experiencing symptoms as a result.

The stiffness that you may be experiencing can result from the deterioration of the lubricating areas, such as the lumbar discs, which would normally cushion movement. Imagine a door which has been opened and closed continuously for 50+ years. Over time, the oil which greases this movement (like our cartilage) is worn away. This leaves nothing to protect the connecting parts of the hinge as they move back and forth. These parts are left to grind against each other, wearing away the supportive structures (of our spine in our case) which causes us pain and limits our capacity for movement.
Another form of arthritis, called rheumatoid arthritis, may also be responsible for the conditions causing sciatica. Rheumatoid arthritis is an autoimmune disease, whereby the immune system erroneously attacks the joints, causing the destruction of these mechanisms.
The onset and progression of spinal stenosis, as a result of rheumatoid arthritis, is rarer as rheumatoid arthritis tends to prefer to attack the peripheral joints. Inflammation and swelling are often present when rheumatoid arthritis is to blame.
#2 – Exercise
Exercise can be your friend or your foe when it comes to sciatica prevention and/or healing. Unfortunately, exercise can also prompt the onset of sciatica.
When sciatica pain is present, it’s best to stay away from strenuous or extended exercise, given the extra strain this may put on your sciatic nerve or on the structures surrounding it. Let’s have a look at why some of the main exercise categories can cause or worsen sciatica:
Weightlifting
Good form is vital when weightlifting, when performing any weightlifting move, you must prevent hyperextension by ensuring you are not rounding your back to prevent sciatica. However, when sciatica pain is present, you must avoid lifts that exacerbate strain on the spine and the sciatic nerve, such as bent-over rows, good mornings, deadlifts, and squatting. Adding weight to these movements increases the pressure placed on your lower back, causing strain to your sciatic nerve.
Many lifting movements require you to bend down. These lifts target the hamstrings and the back. However, the sciatic nerve runs down your back and down the hamstrings; when we bend over or down, we are putting a stretch on the spinal cord, which in turn stretches the sciatic nerve. It is important to know: nerves HATE to be stretched.
When sciatic pain is present, I usually recommend avoiding heavy weightlifting altogether to prevent unnecessary strain. Here is a guide to exercising properly with sciatica.
Core Exercises
A strong core can do wonders for preventing sciatica, as strong back muscles offer greater support for the spine. However, the myth that a “strong core” solves all back problems has infiltrated the field of physiotherapy. Back pain and sciatica run far deeper than just core muscle weakness, as we’ve explored.
“Strong core” exercises can often cause damage which trumps any long-term benefit. Core exercises are notoriously “jolty”. Crunches and sit-ups jolt the spine, putting pressure on the sciatic nerve which provokes pain. Exercises which target the obliques, the muscles running down the side of our abdomen, should also be avoided. These exercises, like russian twists or windshield wipers, involve twisting which puts stress on the vertebrae and compresses the sciatic nerve.
I have found that when people with back pain and sciatica did lots of core work, even if they were able to completely isolate the muscles most involved in supporting posture, they still saw no real improvements. Most worryingly, I also saw that individuals who focused on core training and ended up working out their other abdominals, exacerbated their back pain.
Exercises where both legs are off the floor must be avoided too. These exercises, such as double leg lifts and leg circles, shift all weight into your lower back which will increase sciatica pain and puts you at risk of disc herniation.
For a greater explanation of why core exercises can aggravate sciatica pain, check out the following article.
Extreme, high-impact, team, and racket sports
The clue is in the title: extreme. High intensity sport often involves jarring, twisting, bending and overall unpredictable movement which puts sharp pressure on your spine and sciatic nerve. Overall, any sport, “extreme” or otherwise, that involves a lot of twisting and rapid body contortions should be avoided.
Same with team sports such as rugby and football, which require agility and unpredictable movement that can jar the spine. Racket sports are another nemesis when it comes to sciatica.
As we addressed with Russian twists, rapid twisting of the torso can easily aggravate sciatica, making tennis and squash particularly dangerous.
Golf and hockey compromise the spine during hunching over, with both sports requiring powerful swings which rapidly twist the spine and jolt the sciatic nerve.
When it comes to exercise, it’s best to start with smaller steps, and focus on staying active, before gradually build up intensity and endurance. Like I said before, exercise is incredibly important when dealing with sciatica, but it is essential to choose exercises and stretches which help the pain, not exacerbate it. So, stay away from the bull riding for now!
For guidance on the best exercises to help with sciatica pain, please check out the following article.
#3 – Injury
Injury is another key catalyst for sciatica; either immediately after the injury or later down the line due to deteriorating damage from injury. As covered in the above section, exercise can result in injury when structures are overexerted, overextended, used inappropriately, not warmed up or cooled down properly and so forth.
Additionally, injury can occur for many other reasons, such as a car accident, a work injury, a fall etc. Any of these can result in damage to your spine, which can induce nerve damage. The necessary treatment and recovery time for sciatica resulting from injury will depend on the cause and the extent of the injury.
#4 – Lifestyle
There is a plethora of lifestyle factors which can contribute to the worsening of our anatomical structures and our overall health. Let’s have a look at some factors that play a part in why sciatica happens.
Weight: Managing our weight is important, as extra weight adds extra pressure to our spine. The greater the load that our skeletal system must support, the quicker we wear down the materials cushioning that structure.

Dehydration: Staying hydrated is incredibly important for your overall health, but it is particularly important for your intervertebral disc health. Drinking at least 2 litres of water per day is essential protect your discs from dehydration. If an intervertebral injury has occurred, drinking plenty of water is a highly valuable facet of recovery, as any dehydration in the injured disc will make the nerve compression worse. Drinking 3-4 litres of water each day is critical for recovery.
Prolonged sitting: If your work requires you to sit for extended periods of time, this can flare up sciatica. Sitting applies pressure to your sciatic nerve, as discussed with piriformis syndrome. Given our working patterns, prolonged sitting is not always avoidable. As such, it is worthwhile investing in an ergonomic chair for your working space, or contacting HR to look into adjustments for your working environment to prevent sciatica from occurring.
If you’re struggling with pain or mobility restriction, it is important to address your overall health, as this is typically the first area that contributes to why sciatica happens.
If you’d like some tips on how to improve all aspects of your health, stave off injury and treat problems like sciatica and arthritis, you can grab a copy of my brand-new book, Thriving Beyond Fifty. You can see more details below:
Top Tip: Grab a copy of my #1 Best-Selling book, Thriving Beyond Fifty for more health, wellness and recovery strategies!
Click HERE to view the book on Amazon (UK)!
Click HERE to view the book on Amazon (USA)!
Summary
This article provides a thorough explanation for why sciatica happens and provides details about all of the conditions that can lead to this problem. With any case of sciatica, we always recommend a thorough assessment from a qualified professional.
What did you think of this article? Was it useful? If so, leave a comment below!
The information on Overcome Sciatica is not to be taken as a substitute for medical advice.