Spinal stenosis may or may not be a term you are familiar with. But you may be familiar with the following:
- Back pain and/or stiffness that gets worse the more you move
- Aching pain in your legs as you walk
If these are the symptoms you are suffering with, and you are over the age of fifty, spinal stenosis may be to blame. In this article, we are going to explore what spinal stenosis is and explain the spinal stenosis symptoms, causes and treatment.
First, we need to understand a little about the anatomy of the spine to appreciate what spinal stenosis is.
The spine is made up of 24 movable bones called vertebrae. Each of these bones are separated by an intervertebral disc, made of an outer cartilage shell with a fluid centre, which acts as a cushion to absorb the impact of movement and prevent the vertebrae from grinding against each other.
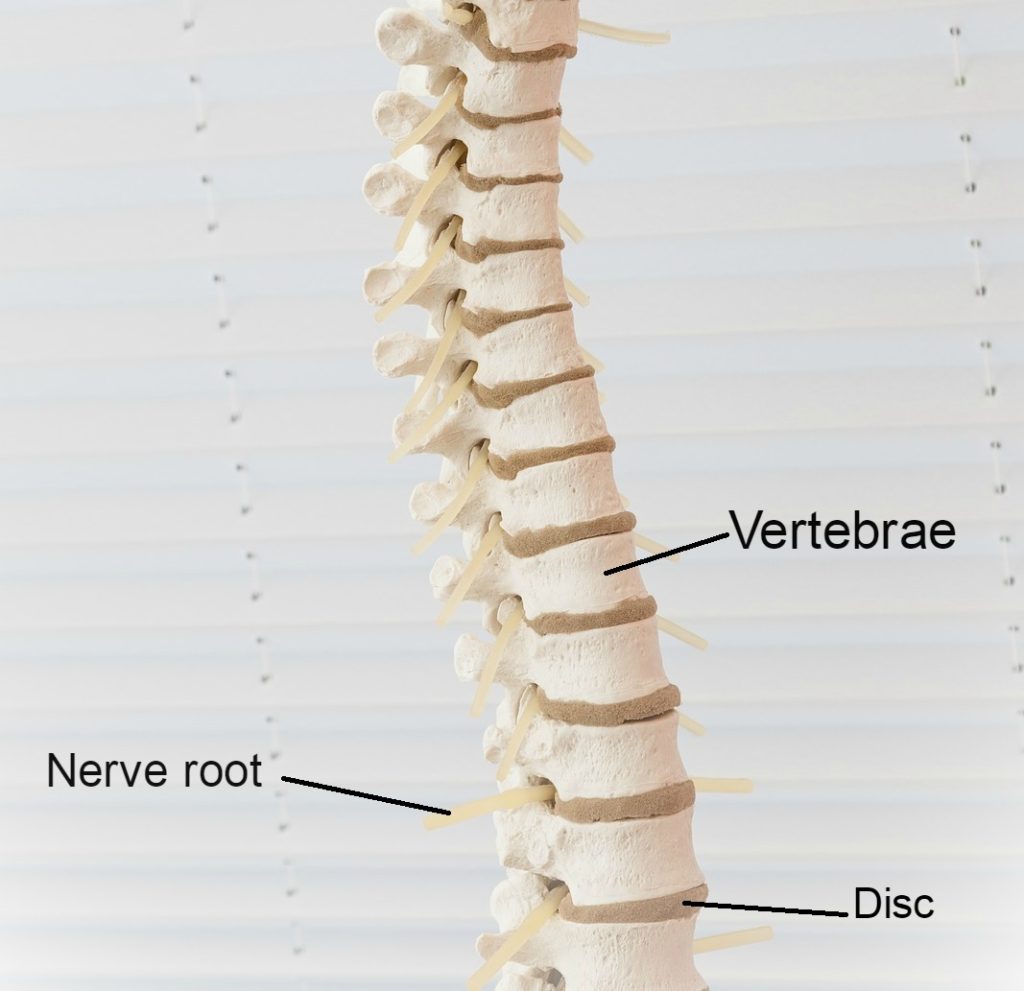
The spine not only functions to provide structure for our body, offering support for the body to complete movement, but it is also responsible for housing the spinal cord.
This “house” is called the spinal canal – a tunnel through the spine through which the spinal cord runs. The spinal cord runs from your brain all the way down to the bottom of your back, supplying nerves throughout your entire body.
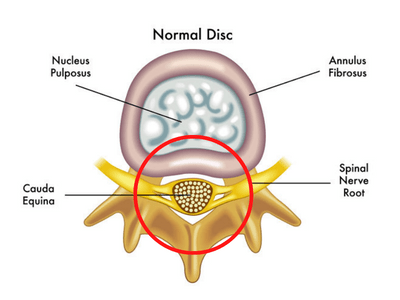
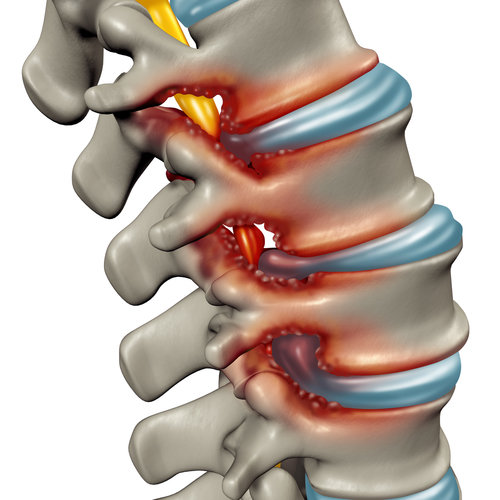
Stenosis refers to the narrowing of a body channel – in this case, the spinal canal. As the spinal canal narrows through the process of ageing and arthritis, it compresses against the spinal cord and pinches the nerve roots. This can be highly painful as nerves are incredibly sensitive.
Stenosis can be localised to one area or globalised throughout the entire spine. Globalisation of stenosis, meaning a widespread narrowing of the spinal canal experienced throughout the entire spine, is called “True Spinal Stenosis”.
Onset of spinal stenosis is most frequently witnessed in the lower back (the lumbar area), given this area often sees the most wear and tear over time and is the area most frequently recruited for movement.
Now that we’ve covered the basics, let’s explore the symptoms, causes, and treatment options for spinal stenosis.
Symptoms
So, how can you identify whether you are suffering from true spinal stenosis? Well, it’s not always easy, as many conditions can share symptoms with spinal stenosis; conditions such as a bulging disc, a herniated disc, peripheral artery disease and more.
“True” spinal stenosis is categorised by the presence of the following 2 symptoms:
- Back pain that is worse when walking and standing, but goes away when you sit or lie down.
- “Neurogenic claudication” – a term to describe a throbbing, dull ache in the lower legs (usually calves) that continues to worsen as you walk and stand, but goes away when you sit down.

The following are also symptoms of spinal stenosis:
- Pins and Needles/Numbness: Spinal stenosis can cause sensory changes in the leg and foot. Usually, the funny sensations will be present in the foot and toes and for some people this symptom can be worse than the pain. This symptom happens because the reduction of space in the spinal canal causes the surrounding structures to press against the nerve in the spine, stopping the nerve from doing its job correctly. This means that some signals don’t get through properly and sensation isn’t felt normally.
- Sciatica: Your sciatic nerve is the largest in the body, running from your lower back and down through your legs. Compression of the passages where the sciatic nerve roots run can cause the pain known as sciatica.
It is always worth being seen by a medical professional if you are suffering from any of the above symptoms. However, if you experience any of the following, you should seek urgent medical attention (list not exhaustive):
- Loss of control over bladder or bowel function
- Loss of sensation or increasing numbness throughout your arms or legs (if a nerve is compressed for too long, it can cause permanent paralysis)
- Severe or intensifying pain and weakness spreading through one or both legs, which restrict your ability to move or stand
Here are some common features mentioned by sufferers of spinal stenosis:
- Pain in the legs when walking that goes away as soon as you sit down
- Total relief of pain when walking and leaning on a shopping trolley
- Difficulty standing up straight or feeling like you want to bend forward when walking
- Aching in legs that gets worse with increasing walking distance
- Difficulty reaching overhead
- Difficulty lying flat and needing pillows to prop up in bed
Spinal Stenosis and Walking Problems
Walking problems are the most common complaint of spinal stenosis. Back pain and calf pain are the most commonly reported walking problems with spinal stenosis.
The reason why spinal stenosis causes walking problems is largely due to the effects of gravity working on the spine as we walk, causing a slow increase in the compression on discs, joints and vertebrae. In a healthy spine, this is totally pain-free, but in spinal stenosis this effect of gravity also leads to a low-level compression on the nerves in the back, causing back pain and calf pain.

For most people who have walking problems with spinal stenosis, simply sitting down can alleviate the symptoms. Another alternative is using a shopping trolley or a walking aid to allow you to lean forward, which will also relieve the symptoms of spinal stenosis when walking.
Causes
It is helpful to discuss how spinal stenosis begins and progresses to understand how the problem deteriorates. Spinal stenosis is not something that occurs overnight.
Ageing is the predominant catalyst for spinal stenosis. It is extremely uncommon for anyone under the age of 50 to suffer from true spinal stenosis. The impact of everyday activity accumulates as we age, leading to spinal “wear and tear”.
Our lifestyle also has an impact on the extent of this wear and tear, particularly for those working physically demanding jobs for long periods of their employment.
Ageing in and of itself is not the root cause of spinal stenosis. Instead, ageing is often associated with the development of OSTEOARTHRITIS, a form of arthritis conveniently labelled “wear and tear arthritis”.
Arthritis is a condition whereby inflammation and/or degeneration is observed at the joints (the areas where two bones meet).
“Osteo-” is the prefix for medical problems pertaining to bones – so, osteoarthritis describes changes to, and degeneration of, bones which form joints.
Osteoarthritis is the most common form of arthritis experienced (ref 1) and the most common cause of spinal stenosis. Osteoarthritis is classified as a degenerative disease, due to the structural and functional deterioration witnessed at the joints.
The following osteoarthritic processes cause spinal stenosis:
- Break down of the cartilage which cushions the vertebrae, causing the bones to grind together
- Development of bone spurs, called osteophytes, on the vertebrae which reduce the space in the spinal canal and compress against the nerves
The stiffness that you may be experiencing can result from the deterioration of the lubricating areas, such as the lumbar discs, which would normally cushion movement. Imagine a door which has been opened and closed continuously for 50+ years. Over time, the oil which greases this movement (like our cartilage) is worn away. This leaves nothing to protect the connecting parts of the hinge as they move back and forth. These parts are left to grind against each other, wearing away the supportive structures (of our spine in our case) which causes us pain and limits our capacity for movement. As such, our movements are made stiff, as they lack the substance which would otherwise help the joints glide.
Another form of arthritis, called rheumatoid arthritis, may also be responsible for spinal stenosis. Rheumatoid arthritis is an autoimmune disease, whereby the immune system erroneously attacks the joints, causing the destruction of these mechanisms. The onset and progression of spinal stenosis, as a result of rheumatoid arthritis, occurs far quicker and often more intensely than when osteoarthritis is observed. Inflammation and swelling are often present when rheumatoid arthritis is to blame.
Roughly 80% of individuals over 55 years old demonstrate evidence of osteoarthritis (ref 2). However, only 60% report experiencing symptoms as a result (ref 2). Therefore, not everyone who experiences wear and tear or osteoarthritis will suffer the symptoms of spinal stenosis.
Wear and tear, and gradual bodily deterioration, is unavoidable. Nevertheless, there are factors that can contribute to the onset of osteoarthritis and spinal stenosis:
- Family history: onset and progression of rheumatoid arthritis can be genetic.
- Sports participation: especially in high-impact sports, sports participation can accelerate the deterioration of the spinal supportive tissue.
- Injury: spinal injury can cause drastic damage or catalyse deterioration of your spine, bringing about spinal stenosis. However, this is more likely to induce spinal stenosis in one area, coinciding with the injury location, rather than throughout the entire spine.
- Your occupation: jobs requiring a lot of physical movement and strain, place your joints under pressure for long periods of time, speeding up the deterioration.
- Your weight: managing our weight is important, as extra weight adds extra pressure to our spine. The greater the load that our skeletal system must support, the quicker we wear down the materials cushioning that structure.
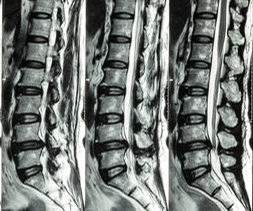
Because of the symptomatic crossover between many spinal conditions, you may be required to have some tests to identify whether what you are experiencing is spinal stenosis. It is worthwhile visiting a medical professional for a firm diagnosis as, unlike a bulging or herniated disc, spinal stenosis is incurable and should be handled uniquely.
To receive a diagnosis of spinal stenosis, the assessment process and tests could include:
- X-ray: allowing the doctor to identify reduced structural space caused by erosion of the cushioning structures and/or growth of bone spurs
- CT scan or MRI: imagining tests which offer more comprehensive insight into structural changes
- Clinical Examination: Usually, there are signs and symptoms that accurately predict spinal stenosis. You might also be examined physically which can reveal a classic stenotic presentation, allowing your healthcare professional to make a diagnosis.
Treatment
When I refer to treatment, I mean measures that can be taken to reduce the symptoms of spinal stenosis – these measures cannot cure spinal stenosis. Unfortunately, the degenerative changes which alter the structure of the spine are permanent, making spinal stenosis irreversible.
However, all is not lost – we can improve symptoms in spinal stenosis, even if we can’t rebuild the physical structures in the spine. I’ve had many testimonials from people with spinal stenosis receiving my treatment and getting a great outcome, as well as new strategies to control their symptoms when they arise. So, it’s definitely worth the effort of finding a proper rehabilitation program if you have spinal stenosis.
Let’s have a look at some of the things that you can do to ease the symptoms and soothe the pain you may be experiencing.
#1 Exercise
Physical therapy is one of the most promising treatments for spinal stenosis. A proper rehabilitation program will help people with spinal stenosis by doing the following:
- Improving the flexibility of the muscles in the legs and reducing the “pull” on the spine so you can walk for further before pain
- Relieving tension in the back muscles and reducing back pain
- Improving fitness capacity so you walk for further with perfect technique, delaying pain
- Improving flexibility in the spine which lubricates the joints that the nerves run through
- Restoring health to the pinched nerves and reducing leg pain
I think the above constitutes a pretty compelling argument for having a good exercise program for spinal stenosis! However, it’s very easy to get it wrong when selecting exercises for spinal stenosis. Please refer to the following article of mine to see the exercises you should avoid to avoid exacerbating your pain: Learn about the spinal stenosis exercises to avoid here!
Now let’s look at some of the best exercises for spinal stenosis.
The common theme for the recommended exercises for spinal stenosis is that they all involve the opposite of spinal extension – we call this movement FLEXION.

Flexion exercises for spinal stenosis tend to bring about a much better outcome than extension exercises. Flexion exercises open up the narrowed spaces in the spine which allows the compressed nerves to “breathe” for a while, relieving symptoms effectively.
The following is a typical exercise program I might prescribe for someone with spinal stenosis. Bear in mind that what I find on my assessment dictates which exercises I might prescribe; some of these exercises may not be suitable for you. Always get an assessment from a healthcare professional before starting any new exercise programme.
The following is NOT to be taken as a prescription; rather, it is just to give an example of a programme that has worked for my clients in the past with spinal stenosis. Be sure to check with your healthcare provider before you begin any new exercise programme.
An Example Program:
Knee Hugs: 10 repetitions on each side; morning, afternoon and evening
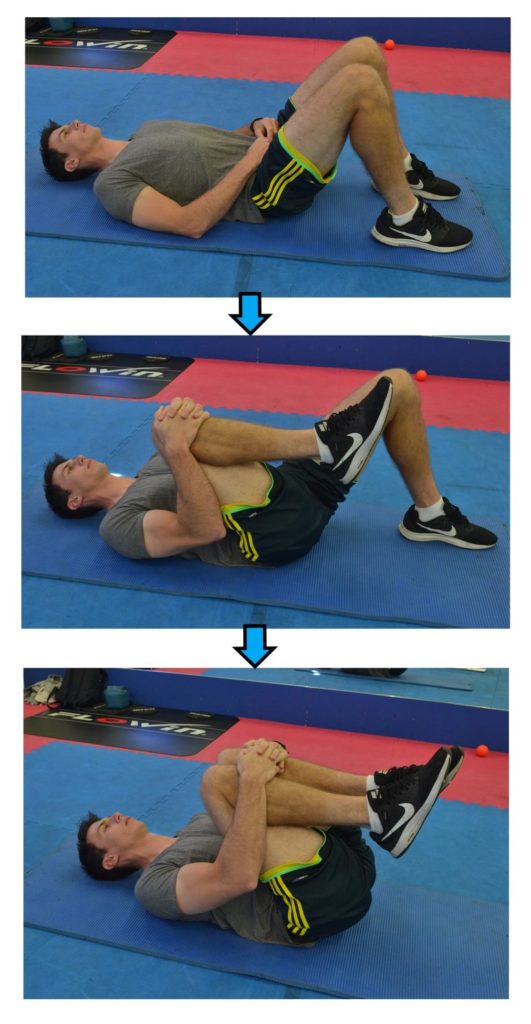
Gluteal Stretch: 30-second hold x 2 each side; morning and evening

Hip Flexor Stretch: 30-second hold x 3 each side; morning and evening

Flexion in Sitting: 5 slow repetitions; morning, afternoon, evening and whenever in pain
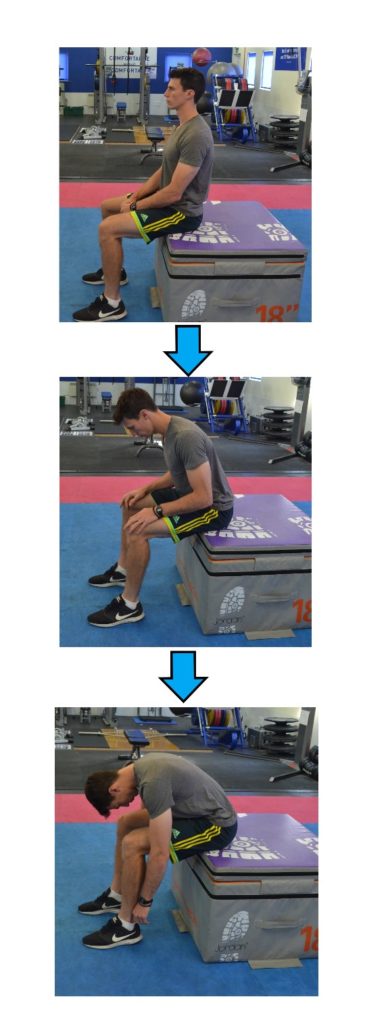
For a full article, with pictures and extended descriptions of each stretch and activity, please check out the following article: Learn the best exercises for spinal stenosis here!
#2 TENS Machine
Many of my patients with spinal stenosis find that a TENS machine can help to relieve their symptoms, when used alongside exercises for spinal stenosis.
A TENS machine works by sending a small electrical signal into the muscles of the back, providing pain relief in many cases, and loosening tight muscles. TENS machines have demonstrated great success with pain relief for sciatica, one of the symptoms of spinal stenosis (ref 3).
Below are my top 3 recommended TENS machines:
Before we dive in, please be aware that we are part of the Amazon Affiliate programme. The following are Amazon affiliate links, so if you choose to purchase a product for your spinal stenosis that we recommend through a link on this page, we will receive a small commission at no extra cost to you. This helps us keep Overcome Sciatica alive! Thank you for your support. Please be assured that we only ever recommend products that we truly believe can help.
1. TENSCare Perfect TENS Pain Relief Machine
This TENS machine has 8 pre-set programmes, so you don’t need to “tune it” yourself – just pick a setting and off you go! There is an option to purchase a ‘Value Pack’ which includes spare pads which I would definitely recommend.
Click HERE to view the TENSCare Perfect TENS Pain Relief Machine on Amazon
2. SHANGPS TENS Machine for Pain Relief
The SHANGPS design has revolutionised the way TENS machines are used for spinal stenosis, meaning you can now get effective pain relief on the go to help reduce the disruption that spinal stenosis causes to everyday life. With its discrete design, you can easily conceal this under clothing and continue with your day-to-day tasks without having to stop and sit down to use a TENS machine for pain relief. Purchase with spare pads for the best value for money.
Click HERE to view the SHANGPS TENS Machine on Amazon
3. TPN 200 Plus TENS Machine
A super-simple yet sleek design, this TENS machine is perfect for those who want a highly effective model and are confident with using a TENS machine for pain relief. This unit doesn’t have a fancy display, so you can customise the settings to best suit your needs, tweaking and changing the frequency until you find one that works best for you.
Click HERE to view the TPN 200 Plus TENS Machine on Amazon
You can also find an entire post I wrote showing you the 10 best TENS machines on the market at the moment by clicking HERE.
#3 Pharmaceutical and Surgical Intervention
There are a range of pharmaceutical options your medical specialist might offer to help relieve some of the pain or discomfort you are experiencing. The following are some interventions and their benefits:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): many NSAIDs are available over the counter, Ibuprofen being the most common. These medications provide pain relief by targeting inflammation which may be causing aches and adding pressure to your nerves. However, your medical specialist might prescribe some stronger or longer lasting NSAIDs, such as Naproxen.
- Anti-seizure drugs: often prescribed to help manage the pain resulting from nerve damage (gabapentin or pregabalin are examples of effective anti-seizure medications)
- Epidural Steroid Injection (ESI): offering powerful pain relief, found to be most helpful for the legs, ESIs are administered to the epidural space which surrounds the spinal nerves.
Alternatively, although we want to avoid surgery, sometimes it may be the only option for relief.
There are surgical treatments which can help relieve symptoms:
- Laminotomy: there are 10 laminae in the lumbar spine. A lamina is a part of the bone surrounding the back of the spinal cord. Partial segments of a lamina can be removed to relieve pressure on the spinal nerves – this is called a laminotomy.
- Laminectomy: In more extreme cases, an entire lamina may be removed to increase the space around your spinal cord. This is known as a laminectomy (or decompression – which describes the reversal of the nerve compression).

#4 Focus On Improving Your General Health
If you’re struggling with your mobility due to spinal stenosis, one thing that might help is to address other general health issues like your weight, your diet, and your general exercise.
If you’d like some tips on how to improve all of those aspects of your health, stave off injury and treat problems like arthritis, you can grab a copy of my brand-new book, Thriving Beyond Fifty. You can see more details below:
Top Tip: Grab a copy of my #1 Best-Selling book, Thriving Beyond Fifty for more health, wellness and recovery strategies!
Click HERE to view the book on Amazon (UK)!
Click HERE to view the book on Amazon (USA)!
Summary
Spinal stenosis can be uncomfortable and incredibly painful. As spinal stenosis is a degenerative condition, its irreversible nature can be very daunting. Remember, you are not alone – many people are experiencing the same thing. Make use of specialists, such as I, and the experience we have to offer to reduce your suffering!
Finally, if symptoms worsen, please seek urgent medical advice to prevent further damage.
References
1 https://www.nhs.uk/conditions/osteoarthritis/
2 https://my.clevelandclinic.org/health/diseases/5599-osteoarthritis
3 https://www.nhs.uk/conditions/transcutaneous-electrical-nerve-stimulation-tens/



